Photos: Danny Wilcox Frazier/Redux
Tanisha Ammons lives on the west side of Chicago in a rented four-bedroom apartment. The neighborhood is working-class. The street is reasonably quiet. The apartment’s not far from the local elementary school, and it’s an easy drive to Midway Airport, where Cornelius Cook, Ammons’ husband, works the night shift. When he leaves for the airport, Ammons—who works by day as a nursing-home aide—lies in bed, listening for the sound of her four sons sleeping. For many parents, this is the day’s most peaceful time—a hard-won silence in which you can hear yourself think again. But for Ammons, bedtime is often its own harrowing beginning.
Sometimes it’s Jacquez who starts. He’s the oldest at eight, a devotee of Spider-Man and Harry Potter, a sensitive kid who writes poetry. In the hours after midnight, Jacquez begins coughing. It’s slow at first and then revs up, until the boy is sputtering in machine-gun intervals. Then it’s Marcus, who is seven, chiming in with his own cough—a raspy hack that can go on for hours. Ammons listens to it almost nightly now, this haunting call and response between the two brothers. Marcus’ cough has grown especially scary in the last year. “It sounds like he’s choking,” Ammons says. “He barely sleeps.”
Nor does Ammons, who gets up and gives the boys cough syrup or a puff of Albuterol, or occasionally just stands in their doorway to make sure they’re all right. On a bad night, her other kids join in. Semaj, the four-year-old, coughs so violently that she doesn’t even bother putting him in his own bed much anymore, preferring to keep him next to her, to make sure he doesn’t turn blue. Omarion, who is two, has a chronic cough as well. And then there are the really bad nights, when the Albuterol doesn’t help and one of the boys—usually Marcus—starts struggling to breathe. This is when he has to be raced to Cook County Hospital’s emergency room, where he’s given drugs to release the invisible stranglehold on his airways. When it’s over, and the boy is breathing normally again, Ammons relaxes—but only for a while: Marcus’ symptoms usually return within days. “I never stop worrying about it,” she says.
On a late fall Thursday, the streets slick in a light drizzle and the last of the season’s leaves dropping wetly from the trees, Ammons and Cook have brought the two oldest boys for a doctor’s appointment in an unlikely spot—a 35-foot-long recreational vehicle parked outside the boys’ school, Webster Elementary. In appearance, the RV is not much different from what a pair of footloose retirees might drive to Yellowstone but for the words “Asthma Van” emblazoned emphatically in black on each side.
All four of the Ammons boys have been diagnosed with asthma, which is to say that their airways are chronically inflamed. When an asthma patient is exposed to certain “triggers”—like changes in air temperature, dust mites, or smoke, among a host of other things—the lining of those airways produces extra mucus, causing them to constrict, which in turn can lead to coughing, wheezing, and difficulty breathing. The feeling is sometimes compared to breathing through a straw. A severe asthma attack can quickly starve the lungs of oxygen. According to the National Institutes of Health, more than 5,000 Americans die this way every year. In Chicago, where the condition is particularly rampant, rates of hospitalization for asthma are twice the national average.
Asthma tends to run in families, which may make it seem like the Ammons children are experiencing little more than genetic bad luck. But genes alone can’t account for the fact that asthma has become the most common chronic illness among children in this country, affecting some 6 million kids, and its prevalence is growing at a rate that some public health experts find alarming. Since 1982, according to the National Center for Health Statistics, the number of asthma sufferers in the United States has doubled.
The progression of the disease is both baffling and frustrating: In recent years, medication used to treat asthma has grown more refined and effective, and the consensus among doctors seems to be that, when properly treated, it should be easy to control. Nonetheless, a December 2004 study by a coalition of health groups showed that nearly a quarter of children with asthma made at least one trip to the emergency room in the past year, and just over half had missed some amount of school or daycare.
Asthma is now the most common reason children in Illinois end up hospitalized, and it’s the leading cause of illness-related school absenteeism nationally. The fallout is significant: Parents miss work to care for their children and scramble to pay hospital bills; children’s grades fall off, and they consistently report feeling socially isolated. One study estimated that childhood asthma costs the nation $3.2 billion annually in health care expenses. All this begs the question: If asthma attacks are largely preventable, why aren’t more of them being prevented?
Inside the Asthma Van, Sandra Peña, a jocular nurse with vivid brown eyes and gigantic hoop earrings, ushers Tanisha Ammons to a seat in the vehicle’s cramped kitchen area. Colorful medical diagrams—of lungs, alveoli, nasal cavities—are hung up on one wall. The cabinets have been stuffed with cartons of inhalers (used to pump medication into the lungs) as well as spacers (plastic holding-tank devices that make it easier for kids to use inhalers), most of them donated samples from pharmaceutical companies. Peña hands Marcus a coloring page and some crayons, while in the back, the van’s driver, Joe Geraci, measures Jacquez’s pulmonary function by having him exhale into a tube that’s been hooked up to a laptop computer. The mobile clinic’s resident pediatrician, a petite, energetic woman named Karen Malamut, reads through the boys’ medical charts.
When Peña asks Ammons who else in the extended family has asthma, she shrugs. “I have it. My sisters have it,” she says. “All the cousins have it. My grandmother—oh, and my mom just found out she has it, too.” She gives a wry smile and shrugs again. “Pretty much everybody’s got it.”

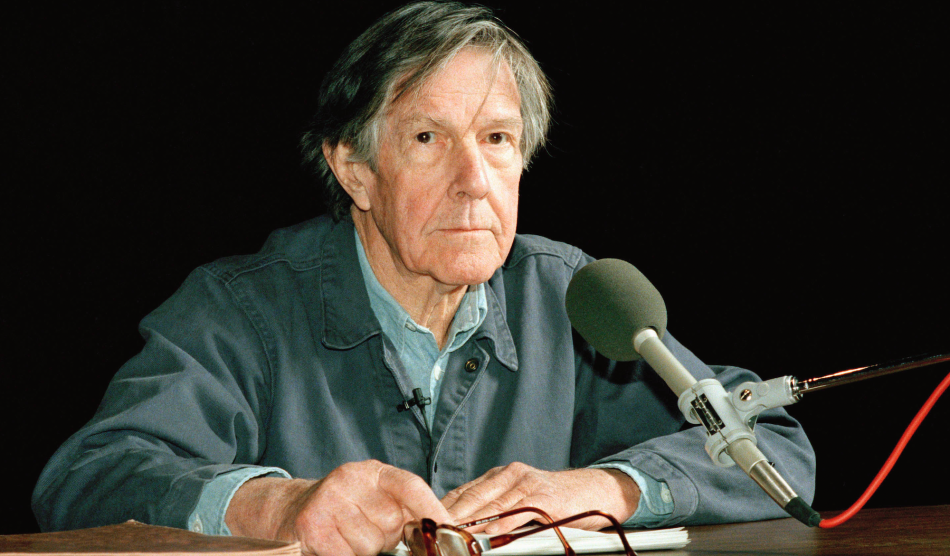
A technician at Cook County Hospital gets Esosa lined up for a lung X-ray.
Health experts are divided on the question of why the number of asthma cases is increasing. Some doctors view the higher rates of asthma as a byproduct of more consistent screening and diagnosis over the past several decades. Others, however, believe that asthma is becoming more frequent and severe due to various environmental changes — many of which are beyond a patient’s immediate control. Asthma has been linked to air pollution and high ozone levels. Pollutants in indoor air — from chemicals used in cleaning products, paint, and pesticides, to dust, mold, rodent and insect droppings, and pet dander — may also bring on asthma attacks, particularly in newer, better insulated homes, which “breathe” less than their predecessors. Stress can exacerbate the disease. “Asthma is so multifactorial,” says Robert C. Strunk, a professor of pediatrics at Washington University School of Medicine in St. Louis. “It’s not a straight line between any one thing and the disease, which can make it very difficult.”
Malamut and Peña spend most of their time on the Asthma Van trying to unravel their young patients’ lives—from what’s triggering the asthma to why a child may not be getting proper medication. Peña gently grills parents for information about the family’s housing—whether, for example, a child sleeps in a basement room, more prone to be moldy, or whether there are many stairs to be climbed, which can be trying for an already challenged set of lungs. She asks whether anyone smokes in the house, and if she doubts the response she may lean over and sniff a parent’s clothing.
Over the course of a 90-minute appointment with Marcus and Jacquez, Malamut and Peña learn that Marcus’ prescription for steroidal nasal spray—which the boys’ mother says eased his symptoms immensely—ran out months earlier, and that Medicaid would not cover a refill. Jacquez, it turns out, has been using his Albuterol inhaler incorrectly, shooting the medication straight into the air rather than into his lungs. Malamut gives him a new, accordionlike spacer to better direct the drug and makes him practice with an empty pump to be sure he’s getting it right. When he does, the eight-year-old beams with pride. “I need this,” he says almost giddily, waving the new gadget for all to see.
Malamut then writes Marcus a prescription for an alternative nasal spray covered by Medicaid. She draws a careful, color-coded illustration to show who should receive which medicine and how often. She explains to Ammons why the cough syrup she’s been giving the kids does nothing to help asthma, then bestows a warm hug upon each boy and makes them promise they’ll return for a checkup next month. Ammons and Cook, openly gratified, usher the kids down the van’s steep steps and herd them across the wet pavement to school.
“My goal is to have every child live as normally as possible, to show them how good it can feel just to breathe the way other kids do,” says Malamut, watching the family go. “Maybe now they’ll get some sleep.”
BEFORE GOING TO RIDE on the Asthma Van, I confess I hadn’t given much thought to the impact of the disease. My brother has had it since he was a teenager, but his is a case of exercise-induced asthma, surfacing only when he works out and handily kept under control with occasional puffs on an Albuterol inhaler. His asthma hasn’t stopped him from running marathons or even from climbing Mount McKinley. Asthma has never seemed like more than a nuisance to him.
More recently, though, asthma has become an issue for friends of mine, a few of whom were introduced to it through unexpected, white-knuckled drives to the emergency room with their children gasping for breath in the backseat. This is when asthma started to seem scary. Still, the children recovered, and their parents—who, like me, have the privilege of good health care and a stable income—have armed themselves with inhalers, nebulizers, and a new mandate to obsessively patrol their homes for allergens that might trigger an attack. But there were enough of these kids that I began to wonder: What’s bringing this on?
One unsettling theory is that the asthma epidemic is at least in part a product of global warming. Last year, researchers at Harvard and the American Public Health Association released a report showing that rising temperatures deliver a devastating one-two punch to asthma sufferers. Warmer weather tends to release more allergens like pollen, ragweed, and mold spores into the air. Exhaust from cars, trucks, and buses, itself a cause of global warming, readily bonds to these allergens, delivering them deep into human lungs. Children, who breathe more air per pound of body weight than adults, are especially vulnerable.
And of all children, no one seems to be more at risk than African American and Latino kids who live in cities. Compared with their white counterparts, African American children in the United States are four times more likely to die of asthma and three times more likely to be hospitalized.
In some Latino neighborhoods, as many as one in three children have been found to have asthma. Why? Air pollution is clearly a factor—in urban areas, it has been shown that children living along bus routes have higher rates of asthma than those who don’t. New research also suggests that the disease may be exacerbated by financial hardship, exposure to violence, and family disruption. And while asthma is clearly a manageable condition, managing it requires patients to have some degree of control over their lives— to be able to get medication and use it regularly, to have periodic checkups, and to elim- inate triggers like dust, pest droppings, mold, and secondhand smoke.
Proof of how hard this can be is found every day on the Asthma Van, which is one of a pair of RV clinics in Chicago run by a nonprofit called the Mobile C.A.R.E. Foundation. Five days a week, the vans park in front of different schools, offering diagnosis, medication, and an invaluable extra—time to talk. (Insurance or Medicaid rules generally don’t reimburse doctors for time spent educating asthma patients, which is key to preventing flare-ups; on the van, Malamut can spend a half-hour or more with each child.) Each van is staffed by a pediatrician, a nurse, and a driver/assistant, and provides an alternative to the emergency room and the storefront medical clinics that offer often perfunctory care to Medicaid patients. In five years of operation, the vans have screened more than 2,600 children for asthma and currently treat approximately 85 children each month. “We could probably have 10 vans operating and still not reach every child in Chicago who has asthma,” says Amy Miller, Mobile C.A.R.E.’s executive director.
On the van, I meet Jamaal Yankieway, a chubby third-grader whose asthma grows worse during hot weather and when he exercises. Even though he is on five different medications, Jamaal spends many summer afternoons pressed up against the window of his apartment, watching other children play outside. “It’s hard seeing him not being able to live like other kids,” says his mother, Tina Williams. “He’ll look out the window and cry because he can’t go out.” Though Malamut believes Jamaal could likely spend more time outdoors without incident, she says a parent’s or child’s fear of an asthma attack can be so overwhelming as to cause its own health problems—such as obesity and diabetes.
There is also Citron Miller, a lanky, handsome nine-year-old boy who is already 5 feet tall and aspiring to a future playing pro basketball. But that dream, as well as any backup career plans, might be compromised by the fact that last year he missed more than 35 days of school because he was having problems breathing. “I’m not working; I can’t,” says his mother, Carmella Miller. Citron’s asthma is easily triggered, she says, by anything from the smell of magic markers to chalk dust, and as a result Miller often wanders through the corridors of his school, checking to make sure he’s okay. “I had two cousins who died from asthma,” she says. “I’m not taking any chances.”
By the time five-year-old Torreon Jackson shows up for an afternoon appointment on the van, his pulmonary function is just 45 percent of what it should be, according to Malamut’s specialized laptop. This is both alarming and entirely ordinary among the children who visit the van. Often, says Malamut, it’s a sign that they are not taking their daily medications — the ones meant to reduce the baseline inflammation of the airways that characterizes asthma. “Because a lot of kids are used to breathing that way, you don’t always recognize that the child is in danger,” she says.
According to Torreon’s mother, Quavelin Jackson, a day earlier when Torreon had trouble breathing in class, his teacher sent him to the water fountain rather than the school nurse’s office, where his inhaler is stored. “I worry that the teachers don’t know what to look for,” says Jackson. “I worry that they might think he’s tired or thirsty and just make him lie down.” Asthma attacks can appear subtle — a child will seem listless or quiet — especially to someone not familiar with the disease. In a nationwide survey released last year, half of school nurses rated staff and student awareness of asthma triggers as “fair” or “poor.”
But the survey gave parents an equally low rating for awareness. After being told the results of his pulmonary function test, Torreon’s mother confesses that she hasn’t been giving him his corticosteroid inhaler daily, as Malamut had prescribed. “I didn’t see how serious it was,” she says, on the verge of tears. This is relatively common, says Malamut, who prescribes two types of medications to most of her patients—a daily steroid that must be administered with an inhaler, and a fast-acting “rescue” medicine (usually Albuterol) to open airways in the event of an attack. Lots of parents skip the daily medication, leaving their children to live with dangerously constricted airways. “A lot of these kids are so used to not breathing, their bodies accommodate,” says Malamut. “But then they’re exposed to one little trigger and that’s it. Nothing can be done to save them.”
Two summers ago, one of Malamut’s patients was a 12-year-old boy she describes as “an incredibly lively, fun, active child.” The boy’s mother skipped numerous appointments on the van, Malamut says, and didn’t always give him his daily medication. When he started gasping for breath one day on the playground, the Albuterol pump couldn’t reverse the tightening of the muscles around his airways. He died before reaching the hospital. “It devastated me,” says Malamut, her eyes welling up. “I know we can’t reach everybody, but he shouldn’t have died.”
Malamut spends much of her time cajoling, lecturing, bullying, mothering, and otherwise reminding parents and kids of how important it is to take their asthma medication regularly. It is basically the only thing she can do to help a family control asthma, as few can afford to make the other changes that might help alleviate the problem. From Malamut’s perspective, uncontrolled asthma creates its own sort of vortex—costing parents precious wages and children valuable schooltime, which in turn diminishes the family’s ability to get away from circumstances that contribute to asthma. “Most of our patients can’t just up and move out of the city or to a better maintained apartment,” says Malamut. “They may need a cat around to take care of the mice, so they can’t get rid of the cat. Or they live in a basement apartment that’s filled with mold, and maybe Grandma takes care of the kids while the parents work, and Grandma smokes like a chimney. Sometimes there’s not a lot a family can do.”
The problem of control comes up again when I sit down with Sylvia Dixon, who is the resident nurse at Webster Elementary School. Dixon estimates that more than half of her time is spent on children who have asthma. Yet that effort is fractured as she, like many nurses working in cash-strapped school systems, is forced to divide her time between three schools, a Head Start program, and a neighborhood center; in total, she is responsible for 1,800 Chicago schoolchildren. “Honestly, I don’t have much time to deal,” she sighs. Nor, she believes, do the parents of the children she sees: “I think the main obstacle is just—life,” Dixon says. “If you’re trying to pay the rent, if somebody’s incarcerated or somebody’s sick, you need to eat. You need shelter. When you’re dealing with all that, asthma is just not a priority.”
ONE DAY A NUMBER of years ago, Lenore Coover, a registered nurse who specializes in asthma management in the Chicago area, was talking to one of her young patients. “It was hot, ozone levels were high,” she remembers. “He’d been having some breathing problems, and the weather would probably cause more problems later. I told him he should go home, close his windows, and turn on the air conditioning.” It took only a minute for Coover to realize that her instructions were ridiculous. “I was telling him to go home, close the windows, and bake!” she says.
Coover calls this her “aha” moment, as it led her to think about how much of the advice medical practitioners give to low-income asthma patients is both well-intentioned and useless. “Doctors will hand a mother a catalog for allergy products and tell them they need to buy mattress covers and pillow covers to get rid of dust mites,” she says. “Well, those things are expensive. It won’t happen.”
Since that time, Coover, a consultant for the American Lung Association and other community health programs, has focused her efforts on training and providing support for a new breed of asthma specialist—not a doctor or nurse, but a $10-per-hour worker who lives within an asthma-afflicted community. Coover estimates there are now 25 or 30 such “community health educators” in Chicago through programs funded by the Centers for Disease Control, the American Lung Association, and other health-advocacy groups. Similar projects have cropped up in New York, Atlanta, and San Francisco.
On a chilly afternoon, Coover takes me to meet Tamara Williams and Janice Patton, two chatty mother-hen types who are known among residents of the Chicago Housing Authority’s Robert Taylor Homes as the “Asthma Ladies.” “We used to be the ‘Condom Ladies,'” says Patton, explaining that they once worked for an HIV-prevention program. “That’s how everybody knew us first.” The condoms, she adds, helped them gain the trust of people who did not like opening their doors to strangers, paving the way for their work with asthma.
Williams and Patton trundle from apartment to apartment paying regular visits to more than 50 families struggling with asthma. They give out caulking guns and steel wool to help plug rodent holes and mattress covers for dust mites—all provided through grants and community programs. They report broken elevators, which force asthma patients to climb multiple flights of stairs, and they write up complaints about demolition projects that get too dusty. Beyond that, they listen.
Both Patton and Williams have lived in the area—a perennially down-on-its-luck neighborhood several miles south of the Chicago Loop—most of their lives. Both have raised children here. And both women have asthma. “There isn’t anything someone can tell me that I can’t say, ‘Girl, I’ve been there, too,'” says Williams, who has 11 children and a bevy of grandchildren to boot. They are also well acquainted with the subtle but insidious effects of chronic asthma: Williams and Patton have both made multiple trips to the ER for their asthma. The resulting ambulance bills, Williams adds, have piled up on her credit report. This is a familiar dilemma for low-income asthma patients. Unpaid medical bills lead to poor credit, which in turn prevents them from owning a home where they might get better control of asthma triggers.
The instability that pervades the lives of people with asthma can produce a vicious feedback loop. One study, by Kathleen Cagney of the University of Chicago, found that asthma was more common in neighborhoods where residents felt a lower level of trust and support. “If you’re in an area where you don’t know your neighbors, you might not feel comfortable letting your kids go outside,” says Cagney. “And when you can’t go outdoors, it really diminishes your health.”
Even in placid suburban neighborhoods, children are spending less time outdoors than they once did, lured by television sets and video games and more likely to be driven from place to place instead of walking or biking. While much has been said about the rising tide of childhood obesity, asthma is arguably its silent partner, a life-altering and often life-threatening disease brought on by changes in our personal and global environment. No corner of the country, no socioeconomic group is exempt.
FACED WITH ASTHMA’S GRIM statistics, physicians and health officials seem finally to be seeking out more creative means for combating the epidemic. Back in 1994, Michael Rich, a pediatrician at Children’s Hospital Boston, launched the Video Intervention/Prevention Assessment project, giving video cameras to 25 children with asthma and asking them simply to film their lives. “The reality is that doctors aren’t going to manage asthma,” says Rich. “It’s the people who have it who have to manage it.” Four years and 489 hours of video footage later, Rich and his staff discovered that more than 90 percent of the asthma triggers in a child’s environment were not reported in the patient’s medical history—a primary tool for diagnosing and treating asthma. The videos revealed mold or old carpeting or pets that hadn’t been mentioned.
“People who have little power to change their lives or their environments—particularly kids—don’t even see the things they can’t change,” Rich says. As a consequence, he insists, treating asthma has to involve more than inhalers and nebulizers. “It’s not just about medicating a pair of lungs,” he says. “It’s about respecting your patients’ lives and getting them to believe that they can take care of themselves.”
In an even more far-reaching experiment, pediatricians at Boston Medical Center in 1993 started soliciting contributions in order to employ a small battalion of lawyers and social workers, who then took on asthma patients’ housing issues, pressuring landlords to address roach problems and repair leaky pipes that may generate mold. This new approach has proved so successful that it’s led to the launch of similar partnerships between doctors and lawyers in New York, Cleveland, San Francisco, and 11 other U.S. cities.
As the day is about to end on the Asthma Van, one last patient climbs aboard. This is Minosha Echols, a bright-eyed first-grader with a sideways ponytail and two missing front teeth. She is dressed in the navy blue pants and white collared shirt required by the school and is accompanied by her mother, Shalanda Johnson. As Minosha takes her pulmonary function test, I sit on the RV’s vinyl bench seat with her mother. “Every day, she was coughing nonstop,” she tells me, describing the weeks leading up to their first visit to the van. “She was choking, almost. And when she coughs, I worry.” She’d taken Minosha to the ER seven or eight times before someone at the school told her about the van.
“She sleeps through the night now,” says Johnson, sounding stunned. “This is the first time in six years she’s done that.” Not only is Minosha happier, says her mother, but she’s gone from flunking her weekly spelling tests to getting straight B’s.
Malamut recognizes the pattern. Once the disease begins to loosen its grip, the results can be far-reaching. Grades improve. Parents can get back to work. Family tensions ease.
“We have a lot of parents who come in and say, I was able to sleep for the first time without worrying, or I was able to hold a job for more than a month,” she says. “I always tell them, when they first come to us, that we can’t change the other things in their life, but we can help their child breathe better.” Malamut smiles. “And sometimes that alone can change a lot.”