Illustration By: Malcolm Tarlofsky
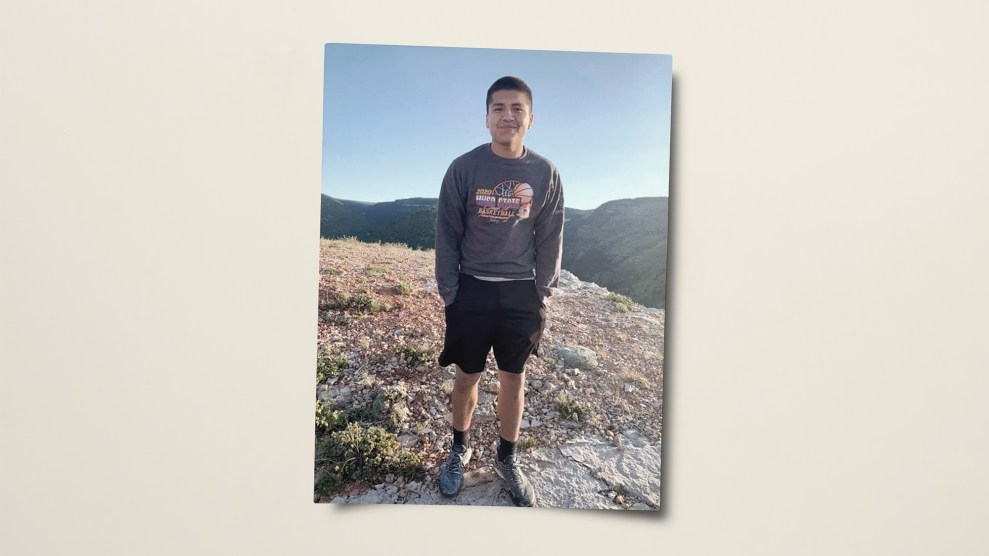
MARIO DELLA GROTTA IS 36 years old, with a buzz cut and a tattoo of a rose on his right bicep. He wears a gold chain around a neck that is thick as a thigh. He’s the kind of guy you might picture in a bar in a working-class neighborhood, a cigarette wedged in the corner of his lip and a shot glass full of something amber. He seems, on first appearance, like the kind of guy who swaggers his way through the world, but that is not true of Mario. There was a time when rituals to ward off panic consumed 18 hours of his day. He couldn’t stop counting and checking. Fearful of dirt, he would shower again and again. He searched for symmetries. His formal diagnosis was obsessive-compulsive disorder, which is just a fancy way of saying scared. Had he remembered to lock the car door? Did he count that up correctly? The French call obsessive-compulsive disorder folie du doute, a much more apt title than our clinical OCD; folie du doute, a phrase that gets to the existential core of worry, a clenched, demonic doubting that overrides evidence, empiricism, plain common sense. For Mario, his entire life was crammed into a single serrated question mark.
Mario’s anxiety was so profound, and so impervious to other treatments, that six years ago his psychiatrists at Butler Hospital in Providence, Rhode Island, suggested psychosurgery, or what—in an effort to avoid the stigmatization associated with lobotomies and cingulotomies—is now being labeled more neutrally: neurosurgery for psychiatric disorders. Medtronic, a Minneapolis-based company, has adapted implants it originally developed to treat movement disorders in Parkinson’s patients for use in the most intractable but common psychiatric problems: anxiety and depression. These neural pacemakers, composed of eight bilateral implanted electrodes, four per hemisphere, emit an electrical current that, theoretically, jams pesky brain circuits, the ones that say you suck you suck you suck or oh no oh no oh no. This idea made sense to Mario. His experience of mental illness was one of a terrible loop de loop. So he said yes to surgery. He said yes in part because he knew that if he didn’t like the neural implants, he could simply have them switched off.
And so, Mario became one of the first American psychiatric patients to undergo this highly experimental procedure. Worldwide there have so far been only some 50 implantations for OCD and 15 for depression, but the technology suggests a not-too-distant future when options other than drugs may be available to sufferers of serious mental illness. Industry analysts predict that the entire “neurostimulation market”—already worth $550 million and growing 20 percent a year—could top $5 billion and that the technology will be adapted to combat everything from addiction to obesity.
Such fervor has critics nervous that rather than curing problems antidepressants have been unable to address, the implant industry could repeat the problems that have scandalized the pharmaceutical world (see “War of the Wires,” page 66). And psycho-surgery, by its very nature, brings with it a thicket of ethical twisters. Whose head is it? By directly manipulating the brain might we turn ourselves into Maytag technicians, programming speed cycles and rinses? Could it be possible to actually control the content of another’s thinking, as opposed to merely their affective states? Even setting aside these sci-fi concerns, should doctors wade into apparently healthy brain tissue when they have yet to precisely locate mental pathology?
THE FIRST RESEARCHER to confirm that brain function, and by extension dysfunction, could be localized was French neurologist Paul Broca, in 1861. Autopsying a patient who could say only one word—”tan”—Broca identified organic damage to what he theorized was the speech center. But it took 75 years, and a Portuguese neurologist by the name of Egas Moniz, to take Broca’s theory of speech localization and apply it to madness. Moniz, who would win a Nobel Prize for his invention of lobotomy, used to stride through the hallways of Lisbon’s insane asylums looking for patients suitable for the frontal lobe surgery, which Moniz’s surgical colleagues performed, first via ether injections, the alcohol essentially burning away the brain, and later with a leucotome, an ice-pick-shaped device with a retractable wire to whisk out gray matter.
In 1936, shortly after the first lobotomies were performed in Lisbon, the procedure came to our side of the sea, where it was adapted with all-American vigor. By the late 1950s, more than 30,000 patients had had lobotomies and the surgery was being used to “cure” everything from mental retardation to homosexuality to criminal insanity. Its most fervent promoter, Dr. Walter Freeman, eventually performed surgeries on multiple patients in an assembly-line fashion. Post-surgery, it was common for a lobotomy recipient to be perpetually placid, a carbon copy of themselves, faint and fuzzy.
While Moniz and his protégés were sawing through skulls, Robert Heath was studying an alternate form of psychosurgery—deep brain stimulation, or DBS—at the Tulane University School of Medicine. Heath took patients culled from the back wards of Louisiana’s mental hospitals, slit open their skulls, and dropped electrodes down deep inside them. With the use of a handheld stimulator, Heath discovered that electrodes placed in the hippocampus, the thalamus, or the tegmentum could produce states of rage or fear, while electrodes placed in the brain’s septal area and part of the amygdala could produce feelings of pleasure. Heath “treated” a homosexual man (identified as B-19) by firing electrodes in his pleasure center while having him watch movies of heterosexual encounters, and within 17 days B-19 was a newly made man. He proved it to Heath by sleeping with a prostitute Heath himself had hired for this demonstration.
Neural implants dramatically illustrated Broca’s notions of localization, and, in so doing, changed the way we thought of the brain. Prior to localists like Broca, people believed thoughts and emotions were carried through the head via hollow tunnels. Now, however, diffuse tunnels were out and in their place, an image of discrete segments, real estate, if you will, some of it swampland, some of it stately, but all of it perhaps subject to human renovation.
And unlike lobotomies, those renovations did not have to be permanent. In a public demonstration at a bullring in Spain, another researcher, Yale’s Jose Delgado, provoked an implanted bull with a matador’s red cape. The enraged animal raced toward him, head down, stopping only at the very last second, when Delgado, with a push of a button, fired the implant and the bull, its aggression eradicated, trotted away. The potential uses and abuses of neural implants were obvious: You could control prison populations; you could effectively wipe out violence.
By the late 1960s, implants appealed to those in the medical and law enforcement communities who believed that urban riots were born not of poverty or oppression but of “violent tendencies” that could be monitored or altered. The federal Law Enforcement Assistance Administration handed out large sums to researchers studying implants and other behavior-modification techniques. Under one such grant proposal, in 1972 Dr. Louis Jolyon West of UCLA was to form the Center for the Study and Reduction of Violence and conduct research at various California prisons. The plan was to take inmates, implant them, and then monitor their brain activity after discharge. When a Washington Post reporter investigated this scheme, he discovered a precedent: In 1968 officials at California’s Vacaville prison performed electrode surgery on three inmates (including a minor) with the assistance of military doctors.
A series of Senate hearings in the mid-1970s brought these and other government forays into behavior modification to the public’s attention, and the public, particularly African Americans, were more than a little perturbed at the thought that mind control was seen as a viable solution to social injustice or crime. Meanwhile, the CIA was rumored to be experimenting with implants to break down POWs and discredit rebellious citizens (Heath admitted he’d been approached by the agency), and Michael Crichton’s The Terminal Man, in which the main character receives implants to control his epilepsy and turns psychotic, became a best-seller.
All this, concomitant with the rise of the antipsychiatry movement, ensured that neural implants fell into disrepute. They were resurrected in 1987 when a French neurosurgeon, Alim-Louis Benabid, operating on a Parkinson’s patient, discovered that if he touched the patient’s thalamus with an electrical probe, the patient’s shaking stopped. A decade later, Medtronic’s neural implants were approved by the FDA for treating tremors, and some 30,000 patients worldwide have since been implanted for movement disorders. But something else was observed. Those implanted Parkinson’s patients, a few brightened right up. It appeared the circuits controlling physical shaking were somehow connected to mental quaking as well. “It’s how a lot of medicine happens,” says neurosurgeon Jeff Arle of the Lahey Clinic in Burlington, Massachusetts. “It’s by extrapolating backwards. Someone then has to have the chutzpah to say ‘Gee, maybe we ought to try this for certain psychiatric problems.’ You believe it’s worth the risk. You don’t know until you try it.”
By the mid-1990s a small, international group of psychiatrists, neurologists, and neurosurgeons was considering using the implants for mental illness. One of their primary questions: Where, precisely, in a psychiatric patient, would one put the electrodes? While Heath and Delgado demonstrated that you can crudely trigger generalized states of affect—like terror and rage—by stimulating areas of the limbic system, no one has so far found those millimeter-sized snarls of circuitry where researchers hope the more nuanced forms of human mental health, or illness, reside. “We want more than anything,” says Dr. Helen Mayberg of Emory University, a DBS depression researcher, “to find that sweet spot, and go there.” Dr. Ben Greenberg, one of Mario’s psychiatrists, notes that it took a long time to hone in on the targets with Parkinson’s. “We are several years into that process,” he says. “We will find the circuitry involved in psychiatric conditions. I think it’s going to happen.”
Some scientists question the very premise that despair can be localized. “Psychosurgery is based on a flawed and impoverished vision of the relationship between brain tissue and psychological disorder. It is extremely unlikely that any psychiatric problem can be located in one so-called ‘abnormal’ brain region,” says Dr. Raj Persaud, a consulting psychiatrist at London’s Maudsley Hospital. “The notion of abnormality remains deeply problematic given the huge overlap between psychiatric and normal populations in all contemporary measurements of brain structure and function. Instead, dysfunction is much more likely to result from a change in relationships between several areas, and so psychosurgery is based on a flawed attempt to carry over the same physicalist thinking that has been so powerful in bodily medicine, inappropriately to the medicine of the mind.”
If finding the exact loci of depression or obsession proves to be problematic, couldn’t scientists simply override people’s psychic pain by stimulating their pleasure centers? That would be too crude, neuroscientists say, akin to getting patients high. Adds Harold Sackheim of the New York State Psychiatric Institute, “If you can get relief without invasive surgery”—this procedure comes with up to a 5 percent chance of hemorrhage; a 2 to 25 percent chance of infection—”you might want to pursue that other avenue first.”
Pills. That’s the other avenue we should supposedly pursue first. And we have. For all our consumption, though, the risk of suicide associated with antidepressants is now considered dangerous enough to adolescents that the FDA has mandated black-box warnings on labels alerting doctors and patients of the dangers. Equally compelling is data that suggests that antidepressants leave a staggering number of users without any relief at all. “We have searched and searched,” says depression researcher Dr. William Burke of the University of Nebraska Medical Center, “for the Holy Grail, and we have never found it.” That’s true. Thirty percent of people who take an antidepressant are not helped by it. Of the 70 percent who are helped, only 30 percent feel robust relief; the other 40 percent get some symptom relief and limp along. Doctors advise the limpers to switch or combine drugs, but between 10 and 20 percent of patients never improve no matter what pills they take.
Mario, who’d tried some 40 different combinations of medications, knows this all too well. He wanted a shot at the ordinary, a lawn he might mow just once a week. The ability to endure the mess and touch of children. He decided the implants were well worth the risk.
ON A MONDAY in early February 2001, as Mario woke up next to his pregnant wife, neurosurgeons at Rhode Island Hospital were suiting up for his operation. A week or so before, Mario had gone to a tattoo artist and had the Chinese sign for “child” inked into his wrist. “If I didn’t make it, if I never got to see my daughter be born, then at least I would have this tattoo,” he says. “Child. With it on my skin, I knew I could go to the grave with some meaning.”
As it is impossible to use animal testing to gauge whether or not DBS can treat depression and anxiety, the only guinea pigs available are people like Mario. To be eligible for neural implants he had to exhaust every available pharmacological option at either optimal or above-optimal doses and undergo at least 20 hours of behavior therapy. He had to understand the risks and implications of the procedure and provide his consent. His case was reviewed by three review boards. The FDA, which regulates medical devices, gave its blessing to this experiment. “We don’t want to repeat the mistakes of the past,” says Dr. Greenberg, his psychiatrist. “We want to be sure this therapy is not only not used indiscriminately, but that it is reserved for the group of people who have failed trials of everything else.”
Once in the OR, Mario was given a local anesthetic. His head had been shaved, his brain targeted to millimeter precision by MRIs. Attached to his head was a stereotactic frame to provide surgeons with precise coordinates and mapping imagery. He’d undergone extensive neuropsychological testing to determine where to put the implants and to provide a preoperative baseline of functioning. After surgery, a DBS patient will be retested with these core questions in mind: Have the symptoms improved or deteriorated or stayed the same? By implanting these electrodes, how has cognitive functioning changed, if at all?
DBS doctors choose their targets—in Mario’s case, the anterior limb of the internal capsule, an area that connects the thalamus with the orbital and medial prefrontal cortex—based on past lobotomies and cingulotomies that were deemed to provide some relief for the symptoms at hand. There is a problem, however, in using past lo- botomy lesions as one’s DBS guidebook: All sorts of surgical lesions have attenuated anxiety and depression in desperate patients, lesions on the cingulate gyrus or the caudate nucleus, lesions to the left or right, up or down, here or there. Without a single sweet spot, the possibilities are disturbingly numerous.
Doctors are anxious to separate DBS from the psychosurgeries of the past, when ice-pick-like instruments were thrust up under open eyes, blades swished through the brain. While the finer points of brain functionality are still hazy, the surgery itself is conducted with far more precision and technological finesse than Moniz or Heath could have ever hoped for. But some facts remain the same. There is a gruesome quality to any brain surgery. The drill is huge; its twisted bit grinds through bone, making two burr holes on either side of the skull.
The drilling was over in a few minutes; surgeons then took a couple of hours to get the implants in place. As is the practice with brain surgery, Mario remained awake throughout and he was repeatedly questioned: “Are you okay? Are you alert?” His head was in the steel halo screwed to his skull. The operating room was cold, despite the relentless surgical sun. The surgeon threaded two 1.27-millimeter wires through the burr holes, wires on which the tiny platinum/iridium electrodes were strung. Picture it as ice fishing. There is the smooth bald lake, the hole opening up, dark water brimming like blood within the aperture, and then the slow lowering of string, the searching, searching, for where the fish live.
Mario could feel none of this because the brain, the seat of all sensation, itself has no sensory nerves. Next the surgeons implanted two two-inch by three-inch battery packs beneath each of Mario’s clavicles and ran wires from the packs (the batteries of which have to be replaced every few months) up under the skin of his neck to the implants. The packs, controlled by a remote programming device, power the electrodes when the doctor flips the switch and adjusts the current. Mario lay there, waiting.
He would have to wait awhile. Psychiatrists do not turn the electrodes on right after surgery. That happens later, when the swelling in the head has gone down, when the bruised brain has had a chance to heal itself and the burr holes have sealed with skin. Then Ben Greenberg would pass a programmer over Mario’s chest, and the wires would leap to life.
AFTER THREE WEEKS, Mario went back to Greenberg’s office. The men sat facing each other, Greenberg with the programmer on his lap. He snapped open the laptoplike device and, using a handheld controller inside, activated the implants. Mario remembers the exact moment they went on. “I felt a strange sadness go all through me,” he says. Mario recalls Greenberg’s fingers tapping on the keyboard, adjusting the current, the pulse duration, and the frequency. After a few taps, the sadness went away. “With DBS the thing has a certain immediacy to it,” says Dr. Steven Rasmussen, Mario’s other psychiatrist. “You can change behavior very, very rapidly. On the flip side of it there’s a danger too. This really is a kind of mind control, you know what I mean.”
This is the rare admission. For the most part, researchers insist DBS has nothing to do with mind control or social shaping; they are simply psychiatrists targeting symptoms. These doctors have seen severe psychiatric anguish and know its remission is always a blessing. But anytime a psychiatrist tries to tweak a patient’s mind, he does so in accordance with social expectations.
Tap tap. Now Mario felt a surge inside of him. Later, outside, Mario peered at the world turned on, turned up, and indeed it did look different, the grass a cheerful lime green, the yellow-throated daffodils. Mario went home. He wanted to talk. He had things to do. Who needed sleep? “You’re like the Energizer Bunny,” his wife said to him. “I felt revved,” Mario says.
Mario is not the only person to become a little too happy on the wire. “That’s one of the dangers,” says Greenberg. Dr. Don Malone of the Cleveland Clinic says, “We don’t want hypomania. Some patients like that state. It can be pleasurable. But this is just like having a drug prescription. We decide how much, when, and how.”
But it’s not the same as with a drug prescription. A patient can decide to take no drugs, or five drugs. A patient can split his drugs with his spouse, feed them to the dog, or just switch psychopharmacologists. Despite prescription regulations, there is tremendous freedom in being a pill popper. But not so for those with implants. True, no one any longer is dragged to the operating table in terror. No one is cut without exquisitely careful consideration. Instruments have been honed, imaging devices advanced. And yet, patients do not, cannot, fully understand, or appreciate, the degree to which, after the surgery, they will be under their doctor’s control. Once a month OCD patients must visit their psychiatrist for what are called adjustments. (Emory’s Dr. Mayberg says that for her depression patients, the rule is “set it and forget it.”) Adjustment decisions, altering the “stimulation parameters,” reflect how the patient scores on a paper-and-pencil test of symptom intensity, and they take into account the family’s and the patient’s subjective report, but the final and ultimately complete control lies with the treatment provider. At a 2004 meeting of the President’s Council on Bioethics, Massachusetts General neurosurgeon and Harvard professor Dr. G. Rees Cosgrove gave a presentation on the issues surrounding DBS. At the end, another Harvard professor asked: “Who holds the clicker?”
Cosgrove’s answer: “The doctor.”
MARIO’S GOOD MOOD continued. He had obsessions and compulsions, but they were smaller now, overshadowed by the grand energy that saturated his existence. For two weeks, he saw Greenberg every day. Greenberg adjusted the settings, turning the frequency, current, and pulse up or down. Sometimes, as a setting was changed, Mario felt that peculiar wash of sadness. Then he evened out.
Six weeks went by. Mario’s daughter, Kaleigh, was born. She was a textbook perfect case of a baby; she screamed, she shat, she drooled, her entire unregulated being
a little vortex of chaos. Mario changed her diaper, saw the golden smear of shit, and in his heart he backed way up. Over the next few months, his mood dipped. He had a terrible time feeding the baby. Sometimes it took him so long to give her breakfast that it would be time for lunch and he’d have to start all over again. The baby, strapped in the high chair, screamed, squash all over her mouth. Wipe that up. Right away. He was better, yes, but not nearly enough.
Mario went back to see Greenberg. Over a span of a few months, with Mario reporting the waxing and waning of his symptoms, Greenberg eventually got the setting right. Mario began to pick up dirty things. It was, at last, okay.
When Mario talks about that time now, tears come to his eyes. “It was like a miracle,” he says. “I still have some OCD symptoms but way, way less. Dr. Greenberg and Rasmussen saved my life. Sometimes they travel to conferences together on the same plane. I tell them not to do it. It makes me very nervous. Who would adjust me if the plane went down? No one else in this country knows how to do it. It’s like the president and the vice president traveling together.”
AT THREE RESEARCH sites in this country (Butler Hospital, the Cleveland Clinic, and the University of Florida, funded to various degrees by Medtronic, the NIMH, and the National Alliance for Research on Schizophrenia and Depression), 15 or so OCD patients have since been implanted. So far, Greenberg and his fellow researchers have seen 50 percent of these patients improve, to varying degrees. Some experience a complete remission, others a more partial relief. In March, Mayberg released the first findings on depression—of her six patients, four experienced complete remission, while the other two derived no benefit at all. “The results for depression are extremely encouraging,” says Mayberg. “We are very excited.”
This excitement, coupled with our growing awareness of psychopharmacology’s
limitations, positions psychosurgery for a potential comeback. After all, when you take a drug you are perhaps altering your brain in ways as or more profound than neural implants do. When you take combinations of drugs, as many psychiatrically ill people do, you put yourself at risk for medication-induced Parkinson’s and a whole raft of other serious side effects. “There is seemingly an advantage to any treatment that can be reversed. However, in the case of DBS this advantage is somewhat illusory,” warns Elliot Valenstein, professor emeritus of psychology and neuroscience at the University of Michigan. “Stimulation on neural tissue is likely to induce long-lasting, and perhaps permanent, changes in neural circuitry and chemistry.” But Dr. Mayberg asks, “How do we know those changes aren’t for the better?” Indeed, researchers hope that DBS might allow patients to better engage in behavioral therapy, eventually making artificial stimulation no longer necessary.
The hopes of implant makers like Medtronic are as big as the market they imagine. They forecast a day when neural implants will treat a wide variety of psychiatric problems, from eating disorders to substance abuse to schizophrenia. “How many people eat too much or don’t eat enough or have some sort of mental illness?” asks Thomas Gunderson, a health care analyst with Piper Jaffray & Co. “There’s a big market out there.” Yet as these devices proliferate, so too will the ethical issues that stick to them like barnacles. Beyond questions of whether a severely mentally ill patient can provide informed consent, there continue to hover fears that DBS could fall into the hands of the state, or the overworked prison systems, and be used as a management device. After all, both of these things nearly did happen in the last century. Neurosurgeon Rees Cosgrove, at that bioethics conference, said, in an effort to caution restraint and thereby prove to the public that times have truly changed, “If we do not do this right and care- fully, and, you know, properly… I do not think we will have another opportunity.”
“It’s easy for any good neurosurgeon to do this now,” Cosgrove added. “That’s the dangerous part—it’s easy.” Even now, no formal regulations prohibit doctors from using Medtronic implants for psychiatric purposes. And whether or not a particular device or usage has received FDA sanction means little anyway. Drugs are used all the time for “off label” purposes; so too could surgery. What will stop neurosurgeons both mercenary and curious from performing these operations on a public clamoring for relief? How long until implants are used to treat milder forms of mental illness? To take this its inevitable step forward, what will stop people from pursuing implants for augmentation purposes? Cosgrove described a patient who, after implantation, became more creative.
But perhaps the simplest conundrum is this: DBS for psychiatric disorders is very experimental. There are no animal models of DBS for anxiety or depression, so these forays into the human brain are largely unguided, despite all the high-tech equipment. At the 2004 meeting Cosgrove, who believes the procedure holds great promise, ticked off other issues: There’s no possibility of large-scale, placebo-blind trials. Thus far Medtronic is the only maker of brain implants, and the major funder of the investigational studies. There’s a risk of infection, of equipment malfunction. Most importantly, Cosgrove said, “We don’t understand how deep brain stimulation works.… We are not clear what the optimal targets are. We don’t even know what the optimal stimulation parameters are, and we don’t know what the long-term effects are…it’s not as simple as we make it out to be.”
But for Mario, it is simple. “I’ve had a hard life,” he says. “My parents got divorced. My father died. I broke my foot. I have OCD.” He pauses. “But,” he says, “I have been helped.”
BACK IN THE 1950S, Rune Elmquist and Ake Senning developed the first implantable cardiac pacemaker, which made some people nervous, suggesting, as it did, an ever-diminishing gap between technology and the soul. Now, pacemakers are as common as grass. Perhaps there will come a time when neural prosthetics will be just as banal, when we will view the brain and its surgical manipulations without awe and hand-wringing.
And yet in no other place is there the potential for a surgeon to so acutely and immediately make memories evaporate, dreams rise, fingers freeze, hopes sputter. The argument could be made that we are not entirely our kidneys, but that we do live entirely within the circle of our skulls.
For Mario, this is all armchair philosophizing, irrelevant to his situation. “I don’t care what it means,” he says. “I care that I’m better. I’m not all better, but I’m better.” So much better that recently he’s let the batteries to his implants run down, though whether this indicates a DBS cure or just an OCD remission, Dr. Greenberg says, it is far too soon to tell.
Either way, Mario is proud of his progress. His wife recently gave birth to a second child. He carries with him pictures of his four-year-old daughter, Kaleigh, who wears tiny gold hoops in her ears. She and Mario play “tent” in the morning, climbing under the quilts, where he shows her shadow puppets. A bird flies. See, a spider. This is the chapel, this is the steeple, open it up, and here are the people. His wife showers; water hits the walls with a sound like static. Outside, cars roar on the roads. Under there, so close to his daughter, Mario can hear her breathe: He is not afraid to hold her hand. Some might say Mario, with his implants, has agreed to a strange sort of bondage, but Mario doesn’t think so. He would say he’s been freed.