Waltraud Grubitzsch/DPA via ZUMA
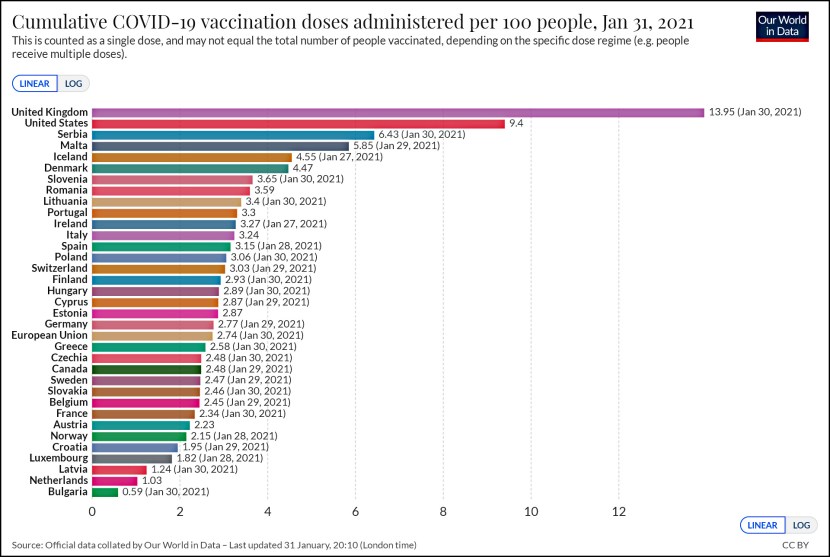
Dan Froomkin has a question:
I made this chart from this data https://t.co/OojDFkptL4 and unless I screwed it up it should freak you the fuck out. It’s for the first two weeks of April We’re not testing more every day. We’re testing less. Why isn’t this top of mind? pic.twitter.com/aYIRBrXmO7
— Dan Froomkin/PressWatchers.org (@froomkin) April 14, 2020
The answer, it turns out, has little to do with the CDC test anymore. Labs in the US are now pretty diverse: some use the CDC protocol, some use the WHO protocol, and others use tests developed by private companies. There are plenty of choices.
But even if there are enough test kits to go around, there’s still a limit to our processing capacity. And that’s made worse by bureaucratic hurdles that prevent academic labs from joining in. A recent article in Nature explains:
A Nature investigation of several university labs certified to test for the virus finds that they have been held up by regulatory, logistic and administrative obstacles, and stymied by the fragmented US health-care system. Even as testing backlogs mounted for hospitals in California, for example, clinics were turning away offers of testing from certified academic labs because they didn’t use compatible health-record software, or didn’t have existing contracts with the hospital.
….“There is a misconception that you only need a PCR machine and a PhD — that is 10% of what you need,” says Fyodor Urnov, a scientific director at the Innovative Genomics Institute at the University of California, Berkeley, which launched a testing operation on 30 March, after weeks of challenges. “My life is waking up at 3 in the morning, and thinking of the 24 things that will go wrong today.”
….A new wave of challenges began when the labs reached out to hospitals in need of tests. “The business of American medicine and the way it is organized is astonishingly unprepared for this,” Urnov says. One problem is that US hospitals use a range of software platforms for electronic health records. Many also have strict administrative procedures for setting up accounts with labs, exchanging samples and handling billing, adds Pride. For this reason, several hospitals chose to stick with the commercial labs they’re already working with, say researchers.
In California, the figures are stark: in late March, the state’s health department reported a backlog of almost 57,000 tests. Even so, Urnov says, hospitals rejected an offer of free tests from his centre, funded by philanthropic organizations. “I show up in a magic ship,” Urnov says, “with 20,000 free kits and CLIA and everything, and the major hospitals say: ‘Go away, we cannot interface with you.’”
This sounds like an area that’s genuinely ripe for presidential—or vice presidential—leadership. An emergency declaration would likely go a long way toward encouraging everyone to work together even if it means exchanging Excel spreadsheets via email for a few weeks. Unfortunately, that would require Donald Trump to implicitly admit that testing is not going quite as swimmingly as he’s been saying for the past month. That’s inconceivable, so instead testing will languish until we slowly build up our stock of test devices and slowly increase our daily throughput.
I sure am getting tired of all the winning.