The Food and Drug Administration, sometimes criticized in past years for being too cozy with corporations, has lately come under attack for exactly the opposite failing. A powerful bloc of critics in industry and the Republican Congress is pushing to overhaul the FDA, claiming the agency is too tough on drug companies, unnecessarily inhibiting innovation and delaying the approval of new drugs and medical devices.
Leading the charge is Speaker of the House Newt Gingrich, who has labeled the FDA the “number one job-killer” in the country, and called its head, David Kessler, “a bully and a thug.” Gingrich’s Progress & Freedom Foundation has announced a radical plan to privatize much of the FDA’s oversight of drugs and medical devices. Not surprisingly, the foundation has financial backing from some of the biggest names in the pharmaceutical industry, including Bristol-Myers Squibb Co., Eli Lilly & Co., and Marion Merrell Dow. Glaxo, manufacturer of Imitrex (see main story), has also given an undisclosed amount to the foundation, in addition to contributions of approximately $325,000 to the Republican Party and Republican candidates (including $4,000 to Gingrich) in the last election alone. As a whole, the drug industry contributed more than $1.6 million to the Republican Party in the 1993-94 election cycle.
If enacted, the Progress & Freedom Foundation’s plan will place responsibility for drug development, testing, and review in the hands of private firms hired by the drug companies themselves, while retaining a weakened FDA to rubber-stamp their recommendations. Additionally, the plan limits the liability of drug companies that place dangerous drugs on the market. An interim report on the foundation’s study was released in June; the final version is due out later this fall.
Under the plan, government-licensed firms called DCBs –drug (or device) certifying bodies–would be retained by drug companies to develop, test, and review new products. According to the proposal, “competition between firms would inevitably produce a lower-cost, faster, and higher-quality development and approval process.”
FDA spokesperson Jim O’Hara offers an alternative view: “What this report proposes is dismantling many of the safeguards that protect the public from drugs and devices that are unsafe or just don’t work. This is basically a proposal that says public health and safety are commodities for the marketplace.”
Though drug testing and review would be privatized under the plan, the FDA would still exist and would theoretically have final say on new products. However, the report states there would be “a strong presumption that private certification decisions would not be overturned without substantial cause.” Further, the FDA would not be authorized to request additional testing or data, and it would “have to exercise its veto within a fixed time period (e.g., 90 days) after which the drug would automatically receive FDA approval.”
The Progress & Freedom Foundation plan also limits the liability of drug companies should a patient be injured or killed by a dangerous drug or medical device. According to the proposal, a victim could not sue for punitive damages if the manufacturer of the product could show that it had met regulatory standards–however weakened–during development and testing.
Dr. Sidney Wolfe, director of Public Citizen’s Health Research Group, says the plan to limit corporate liability is “hypocrisy at the very least.”
Even some in the drug industry believe the Progress & Freedom Foundation’s proposal goes too far. Steve Berchem of the Pharmaceutical Research and Manufacturers of America says that while some drug reviews can be handled by the private sector, it would be a mistake to weaken the FDA’s authority over product approvals. “We need an FDA that maintains public confidence,” Berchem says.
Nonetheless, the political writing on the wall is clear. Earlier this year, the FDA announced steps to reform itself, including the creation of a pilot program to allow private companies to review some medical devices. But this compromise isn’t going to satisfy the hard-liners. Progress & Freedom Foundation spokesperson Rick O’Donnell says the FDA proposals “don’t actually hit at the heart of the systemic problems that our plan is addressing.”
As the battle to reshape the FDA heats up in the coming months, the Progress & Freedom Foundation will coordinate its efforts with those of other heavily funded right-wing attacks. But look for Newt and Company to draw their proposals directly from the foundation’s plan.
Despite the medical risks posed by Imitrex injection, you are not required to take the medication in the presence of your doctor. Imitrex can be administered at home, at your workplace, or at any other location by using an “autoinjector,” a futuristic-looking plastic injector that contains a prefilled syringe of Imitrex and requires only the push of a button to release the medicine into the bloodstream.
The autoinjector looks so neat, in fact, that a picture of it was featured in the hip, new technology magazine Wired. “I thought it was a wild-looking device,” says David Jacobs, editor of Wired’s “Fetish” section, where the magazine promoted the product under the heading “Kill Migranes”–spelling error and all. Jacobs discovered Imitrex when a Wired employee who suffers from migraines brought her autoinjector to work. “You have to have an eye for things that just stand out,” Jacobs says. “I look for diamonds in the rough.”
Unfortunately for readers of Wired, the magazine editors didn’t look beyond Glaxo’s nifty packaging job. The autoinjector contains a six-milligram dose of Imitrex, which has been associated with heart attacks, strokes, and other health problems. Glaxo also recommends a second injection as soon as one hour after the first if the migraine symptoms come back. And although the company suggests that the first injection be given in a doctor’s office, that decision is left to the doctor’s discretion. –Andrea Buffa
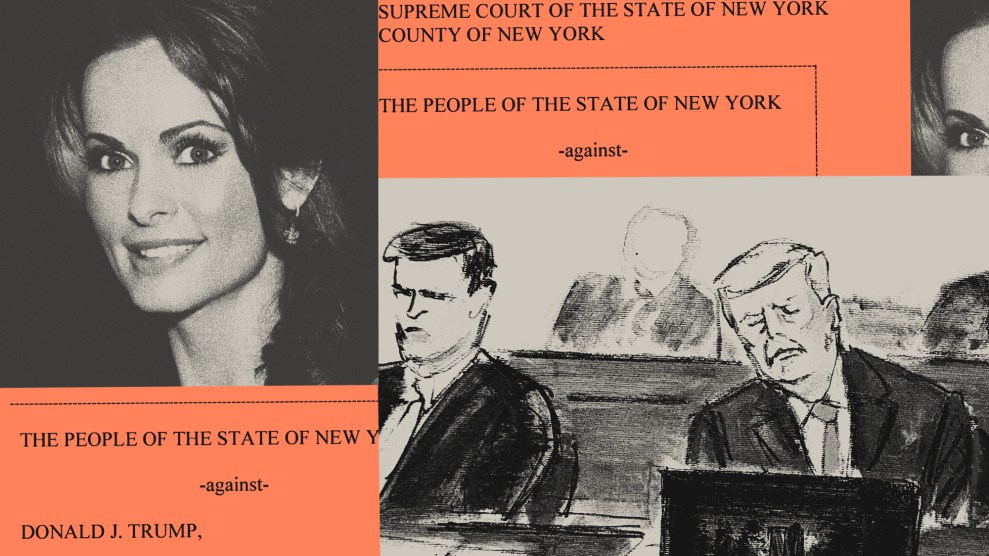
On the morning of Feb. 4, 1994, Dianne Riley joked nervously with her husband and one of her four children about a dream she’d had the night before in which someone had died. This wasn’t a pleasant way to begin the day, because once before Riley had actually forecast a death in this manner.
To make matters worse, Riley had a miserable headache. For five days running, the 41-year-old assistant manager for a Ramada Inn in Kansas City, Mo., had felt the pain in her head build to the point where she would be overpowered by nausea.
Later that morning, Riley had an appointment with Dr. Samuel Ho, a specialist in internal medicine. He diagnosed migraine, a slowly developing headache with throbbing pain that is usually felt on only one side of the head. The condition is believed to affect between 15 and 25 million Americans, mostly women.
Ho recommended Riley try Imitrex, the brand name for sumatriptan succinate, a heavily marketed new drug for migraines. At 12:25 p.m., Riley was given a six-milligram injection of the drug. Within minutes, she began to sweat, vomit, and experience chest pains.
Technicians managed to hook her up to an electrocardiograph and quickly discovered that she had an abnormal heart rhythm. They called 911.
An emergency team reached Ho’s clinic at 12:56 p.m., and transported Riley to St. Luke’s Northland Hospital where she arrived with resuscitation efforts in progress. At 1:58 p.m., a doctor pronounced Riley dead. An autopsy performed the
next day indicates Riley’s cause of death was “a result of adverse effect of Imitrex.”
On April 15, two months after Dianne Riley’s death, her family filed a lawsuit in the Circuit Court of Jackson County, Mo., charging that Glaxo, the British-based manufacturer of Imitrex, had been aware that the drug could cause serious harm or even death. The lawsuit accuses the multinational and its Cerenex division in North Carolina of not adequately labeling Imitrex and not disclosing the drug’s true risks, “in order to collect substantially higher profits.” Glaxo will not comment on the lawsuit because it is under litigation. The case, still in the legal discovery phase, is expected to go to trial sometime in 1996.
Dr. Vincent Di Maio, one of the country’s leading forensic pathologists and editor of the American Journal of Forensic Medicine and Pathology, intends to testify on the Rileys’ behalf. He says he has examined all the microscopic slides of tissues and organs from the Riley autopsy and has no doubt that its conclusion was correct. Although Dianne Riley had some risk factors for heart disease (e.g., smoking, family history of heart disease), Di Maio says her heart and coronary arteries were healthy; the heart attack that killed her was precipitated by Imitrex.
“It is a very complete autopsy,” Di Maio says. “This is a simple case where a young woman took Imitrex, started to react to it badly, developed an irregular heartbeat, and died. The autopsy shows clearly that there was no evidence of hardening of her arteries, no evidence of infection, no evidence of an enlarged heart, no evidence of stroke, no evidence of meningitis or encephalitis, no evidence of a blood clot, no evidence of lung disease, no evidence of asthma or allergic reaction, no evidence whatsoever of disease. If there is no other cause of death, by deductive reasoning she died of a coronary vasospasm following the use of Imitrex.”
Imitrex, a top-line Glaxo drug, is used by more than two million people worldwide. The drug’s sales in fiscal year 1993-94 were $365 million. Both of those numbers are likely to increase when the tablet version of the drug becomes available on the U.S. prescription market this month.
To date, the Food and Drug Administration has received 3,526 voluntary reports of possible side effects, ranging from mild to severe, associated with the use of Imitrex. Included are reports of 83 deaths and at least 273 life-threatening complications.
Earlier this year, Glaxo became the world’s largest pharmaceutical company when it bought Wellcome, another British multinational. Glaxo and Wellcome sold a combined $11.6 billion worth of products last year, to fight everything from asthma and ulcers to heart disorders, infections, and migraines.
In the high-stakes pursuit of competitive advantage, drug giants like Glaxo must sometimes spend hundreds of millions of dollars to develop new drugs. To see returns on these investments, companies push hard to get the drugs through the regulatory approval process and promote them vigorously when they are first released. Glaxo’s push of Imitrex was no exception.
The history of Imitrex goes all the way back to 1972, when Glaxo launched a research program to develop a new migraine drug. The company’s goal was to find a chemical that could narrow swollen blood vessels in the head, thereby stopping the pain of migraine headaches. But it was also important that the drug not narrow or squeeze blood vessels in the heart, because this could cause spasm in those vessels and trigger a heart attack.
More than a decade passed before Glaxo scientists came up with Imitrex. The drug mimicked serotonin, a chemical produced naturally in the body. Serotonin contracts blood vessels by acting on their cells via the gateways or “receptors” known as 5HT. Glaxo researchers thought that Imitrex would affect only the type of 5HT receptor known as 5HT-1, which they believed was rarely found in heart vessels, and therefore the drug would not cause heart spasm.
Glaxo believed it had a blockbuster drug in the making, one with a potential market of hundreds of millions of dollars.
Looking back, however, some fundamental research data contradicted the presumption that 5HT-1 receptors were generally absent from heart vessels. In one small laboratory study, Glaxo researchers found that Imitrex caused small contractions in coronary artery samples from explanted human hearts, indicating the presence of 5HT-1 receptors in heart vessels. An independent study also supported this hypothesis by demonstrating that Imitrex could cause temporary narrowing in the coronary arteries of patients with or without signs of heart disease.
Glaxo, however, emphasized other research that supported Imitrex’s safety. Specifically, one Glaxo study showed that Imitrex did not affect the cardiovascular systems of dogs, indicating that 5HT-1 receptors were not present in the dogs’ heart vessels and suggesting that this might be true for human beings as well. The company also assured regulatory agencies that the drug was safe because its heart-monitoring tests during clinical trials showed that very few patients suffered heart disturbances.
Strong indications that these assurances were hollow first surfaced in Canada.
On Dec. 20, 1991, Dr. Michele Brill-Edwards, then the assistant director of the Bureau of Human Prescription Drugs at Health and Welfare Canada, wrote a memo to the bureau’s assistant director of operations, Peter Jeffs, expressing her suspicion that Glaxo was pressuring one of her reviewers to move faster on getting approval for Imitrex.
After Brill-Edwards reviewed the file herself, she believed that there were potential problems with Imitrex. She was particularly concerned that Glaxo had only thin documentation to show that Imitrex was not a danger to heart vessels.
Brill-Edwards also wondered about Imitrex’s recommended dosage of six milligrams. Glaxo studies had shown that a one-milligram dose was enough for some patients and three milligrams worked for up to 60 percent of patients. Only an additional 10 to 20 percent benefited from the six-milligram dose. Yet contrary to standard medical practice, which recommends tailoring dosage to a patient’s needs, Glaxo recommended six milligrams for everyone. (A Glaxo spokesperson told Mother Jones that the company chose the six-milligram dose as “the best balance between efficacy and safety.”)
For more than two weeks, Brill-Edwards (who is under orders not to discuss Imitrex with the media) raised concerns within her bureau about Imitrex’s safety, and questioned Glaxo’s efforts to expedite the drug’s approval. In a Jan. 7, 1992 memo, she described the situation to her boss, Dr. Claire Franklin, then the director of the Bureau of Human Prescription Drugs:
At 5:15 p.m. [Jan. 6], Ms. Gita Lingam, [then the] head of regulatory affairs for Glaxo, telephoned.a Threatening remarks were made courteously. Ms. Lingam noted that Mr. Randall Chase [then a senior vice president of Glaxo Canada] intends to take the matter “to a higher level” if there are further delays. Legal action was intimated.a
[T]he product monograph remains less than adequate in its characterization of safe usage of this valuable new product. My recommendation is that the clinical division should be required to remedy the deficiencies in the product monograph.–This action should be undertaken notwithstanding substantial pressure to the contrary from the manufacturer.
The deficiencies in the monograph were not remedied. On Jan. 16, 1992, nine days after Brill-Edwards wrote her memo, Glaxo announced that it would construct a $70 million manufacturing facility in Canada, promising more jobs and research spending.
Four days later, on Jan. 20, senior managers at Health and Welfare Canada approved Imitrex.
The next month, when Glaxo launched its promotional campaign for Imitrex in Canada, it claimed the drug “works only on the painfully swollen blood vessels in the head.” The labeling for Imitrex, however, recommended that people with serious heart problems shouldn’t be prescribed the drug, indicating that Glaxo was, in fact, aware of its potential effect on heart vessels.
But when reports began to file in at Health and Welfare about side effects following an injection of Imitrex, Glaxo officials took the public position that these reactions were rare and unexplainable. As of July 1992, Health and Welfare had received only 20 voluntary reports of adverse side effects associated with the use of Imitrex, including severe chest pain and breathing difficulties. But by November, an additional 70 reports had been filed, again including chest symptoms. That month, Health and Welfare and Glaxo quietly cooperated in rewording the product labeling. The new labeling advised doctors to take a careful medical history to avoid prescribing Imitrex to anyone with heart disease.
Meanwhile, in Britain (where Imitrex had been available since 1991), a new chapter in the drug’s story had begun. A case report was published in May of 1992 in the British Medical Journal concerning a 47-year-old man with no sign of heart disease who developed severe chest pain after injections of Imitrex. Further tests with the patient showed that within six minutes of receiving a shot, his heart vessels began constricting. A month after this case was reported, the U.K. Committee on Safety of Medicines, Britain’s drug regulatory group, reported that Imitrex could cause heart vessels to constrict.
Glaxo, however, continued to maintain that severe side effects were rare, and that those patients who suffered heart-related complications must have had some underlying heart problem.
In the United States, the FDA had the advantage of looking at several months’ worth of cases of side effects associated with Imitrex in Canada, Britain, and the Netherlands before deciding whether to approve the drug for the American market. Dr. Paul Leber, chief of the FDA’s Division of Neuropharmacological Drug Products, clearly struggled with the decision. In an August 1992 memo to Dr. Robert Temple, director of one of the FDA’s three Offices for Drug Evaluations, Leber questioned the value of Imitrex, writing that its benefit was difficult to determine because of the absence of comparisons with alternative treatments (such as painkillers, anti-inflammatory drugs, narcotics, and medications derived from a common fungus). “It is particularly difficult to get a clear view,” Leber wrote, “because the product has been promoted worldwide with considerable vigor. Indeed, one expert has privately communicated his belief that the utility and advantages of Imitrex have been considerably inflated.”
Four months later, with Imitrex on the verge of approval, Leber voiced deep concerns about the drug’s safety, particularly for patients who might have undiagnosed heart conditions. In another memo to Temple, dated Dec. 28, 1992, Leber wrote that if the drug is “widely used once marketed, a sizable number of patients with significant, but unrecognized, coronary vessel disease will be inadvertently exposed.a If this occurs, it is probable, if not certain, that some of these individuals will suffer serious harm, even death, following their use of Imitrex injection. In fact, postmarketing reports from countries in which Imitrex is available indicate that such events have already occurred.”
But despite this danger, Leber didn’t want to stop FDA approval of Imitrex. “What counts more?” he wrote. “The rights of millions of otherwise healthy migraineurs to have access to an effective and, for them, safe treatment, or the rights of those who may be inadvertently injured by its marketing?–If there are to be potent drugs like [Imitrex]–society must be willing to tolerate the injury they will cause to some proportion of those who use them.”
The FDA approved Imitrex for sale the next day.
As part of its Imitrex information package to the press, the FDA stated that “people with underlying heart disease should not take the drug because of its potential to cause constriction of coronary arteries.” As a precautionary measure, the agency also recommended that doctors consider giving the first injection in their office to patients who might have underlying coronary heart disease.
But the drug’s labeling included no recommendation to doctors to exclude patients whom they only suspected could be at risk for underlying heart disease. And there was no recommendation for how to treat patients who seemed to be suffering a negative reaction.
Imitrex’s reputation as a breakthrough migraine treatment was largely made in the initial burst of promotion upon its release. It wasn’t until August 1994a20 months after the drug’s approval–that the FDA and Glaxo cooperated in making the first significant labeling change for Imitrex. By this time, the number of reported deaths possibly related to Imitrex had grown to at least 33. A new section was added to the Imitrex label. Titled “Drug-Associated Fatalities,” it discloses that some of the reported deaths had occurred within a few hours of Imitrex’s use and that the drug’s “specific contribution–to most of these deaths cannot be determined.” The death of Dianne Riley is noted, though not by name, among them. (The notation, however, does not mention that Riley’s autopsy showed her to be free of heart disease. Instead, it lists her risk factors for heart disease–“positive family history, postmenopausal woman, and smoking”–implying that she might have had heart disease.) The FDA also asked Glaxo to send out what is known as a “Dear Doctor” letter, to inform physicians of the labeling change.
Three months later, there was a second major relabeling and another Dear Doctor letter. Glaxo now emphasized that Imitrex should only be used when a doctor had clearly established that a patient was suffering from migraine. The drug was not intended for any other kind of headache. The new labeling also recommended that Imitrex “not be given to patients in whom unrecognized coronary artery disease is likely without a prior evaluation for underlying cardiovascular disease.” These patients include postmenopausal women, males over 40, and those with risk factors for heart disease, such as high blood pressure, high blood cholesterol, obesity, diabetes, smoking, or strong family history of heart disease.
Of course, even a patient who does not fit these categories might have undiagnosed heart disease and thus could be at risk for serious Imitrex-related complications. According to Dr. Robert Vogel, head of the division of cardiology at the University of Maryland Hospital, the problem is compounded by the fact that there is no such thing as “insignificant” coronary disease. “So-called insignificant coronary disease can be lethal,” he says.
The most disturbing possibility is that Imitrex may also affect healthy hearts. Glaxo has consistently maintained that in cases like the one described in the British Medical Journal, some early coronary disease must have been present, even if it was never detected. But what does it mean to claim that someone had incipient (Continued on page 70) (Continued from page 31) heart disease if, as in Riley’s case, the patient was outwardly healthy and the disease could not be detected, even by an autopsy? And if the disease is undetectable, how can doctors rule out patients for Imitrex use?
Concerns that Imitrex might trigger heart attacks are not Glaxo’s only problem. Recent research suggests that coronary spasm, such as that apparently caused by Imitrex, can gradually damage heart vessels over the long term. There is also concern that the drug may induce strokes in some patients.
Speaking before an audience of doctors and at least one Glaxo representative in October 1994, Health and Welfare Canada’s Brill-Edwards discussed the potential long-term risks of Imitrex use. She pointed to animal research showing that if coronary arteries are regularly constricted, hemorrhaging in the endothelial tissues will occur and over time may promote clogging of the arteries, increasing the chance of a heart attack. “So, we could be dealing with a scenario where we are giving the drug thinking everything is fine and not realizing that, over years, the risk of atherosclerosis is increasing. We are not even looking for it or monitoring for it.”
To date, the FDA has also received reports of at least 31 strokes (damage to the brain due to interruption of the blood supply) and an additional 53 cases associated with stroke or with conditions that can lead up to stroke.
A lawsuit in Travis County, Texas, is currently in the discovery phase and scheduled for trial this October. On Sept. 1, 1993, shortly after injecting herself with Imitrex, Donna Sue Currie, a dental assistant, suffered a stroke that left her disabled. Her lawyer, Jay Winckler, says the discovery process has revealed other cases of Imitrex-associated stroke known to Glaxo, but he won’t say how many because the case is in litigation.
Dr. K.M.A. Welch, a migraine and stroke specialist affiliated with the Henry Ford Health Sciences Center in Detroit, Mich., confirms that strokes have been reported in association with Imitrex. Welch points out, however, that establishing a causal relationship is tricky, because anyone who suffers from a migraine already has a significantly greater risk of having a stroke. “It is often difficult,” he says, “to determine whether the drug or the migraine itself caused the stroke.” But he adds, “Because Imitrex is a vasoconstrictor, it may well play some role in tipping the balance.”
The FDA’s effort to balance Imitrex’s benefits and risks has two major flaws. First, there is insufficient data to show that Imitrex is more effective than other treatments. More importantly, the FDA, along with Glaxo, has failed to provide potential patients with enough information to make an informed choice about a drug that may pose serious health risks.
According to Dr. Sidney Wolfe, head of Public Citizen’s Health Research Group, a watchdog agency in Washington, D.C., “Imitrex is clearly a drug of last resort, to be used only when everything else fails.”
But that is neither the way Glaxo marketed Imitrex, nor the way the FDA and other regulatory agencies have recommended it. Had Dianne Riley known the risks, she might have decided against taking Imitrex. Had she first been prescribed another migraine treatment, it might have done the job. Had the labeling recommended that her doctor have nitroglycerin on hand in case of heart attack, Dianne Riley might still be alive.
Such a failure on the part of the FDA does not bode well at a time when the agency is under attack for being too tough on drug companies (see sidebar, page 28). If the anti-regulatory assaults of drug industry lobbyists and congressional Republicans result in further downgrading of the FDA’s ability to ensure drug safety, more patients like Dianne Riley may die.
Robert Temple, the FDA bureaucrat responsible for clearing Imitrex for the U.S. market, maintains that, thus far, the drug has been safe. He confirms, however, that there is “theoretical concern about Imitrex’s causing spasm of coronary arteries–[leading] to chest pain and, if prolonged, to a heart attack.”
Temple concedes that doctors might be advised to give nitroglycerin to patients who appear to be suffering heart-related reactions. But he says there was no real need to add this information to the label, because “we thought everyone would know that,” and it might cause “undue alarm.”
Moreover, Temple admits that doctors often cannot determine which patients will suffer heart-related complications, because it is not practical to give them advanced medical tests–and even these might not turn up incipient heart disease. Asked if this means that taking Imitrex is basically a crapshoot, he replies, “Realistically, there is not much you can do about it.”
Dr. Donna Gutterman, Glaxo’s director of medical affairs in the Central Nervous System Division, agrees: “It can be extremely difficult to work up a patient for heart disease.” But she claims that Glaxo cannot be expected to provide doctors with a series of instructions on how best to weed out patients potentially at risk, because the company believes “the physician is in the best position to evaluate the patient.”
Gutterman also confirms that although “it’s difficult to tease apart what might be happening” when a stroke occurs, Imitrex might in theory contribute. She points out that a stroke produces vasoconstriction and “the addition of Imitrex, which is a vasoconstrictor, can worsen the bleeding going on.”
Meanwhile, a universe away from the offices of regulatory agencies and multinationals, Dianne Riley’s husband Lionel remembers her as “a people’s person.” He says that after her death, “a part of me was just taken away.” Daughter Natousha Murray, 25, is furious at Glaxo for running TV commercials that show a woman her mother’s age walking in the park and feeling good because of the company’s new treatment for migraine. “My mother can’t walk in the park and play with her grandchildren,” she says. “It’s sickening to see this commercial.”
Nicholas Regush is an investigative reporter and television producer living in Montreal.