<a href="http://www.shutterstock.com/cat.mhtml?lang=en&search_source=search_form&search_tracking_id=SIPB2mrsFVpbcMy8IY2CXA&version=llv1&anyorall=all&safesearch=1&searchterm=baby&search_group=&orient=&search_cat=&searchtermx=&photographer_name=&people_gender=&people_age=&people_ethnicity=&people_number=&commercial_ok=&color=&show_color_wheel=1#id=134109536&src=hh98cmJ_SA5CrHnV6AqJrg-1-52">Sandrinka</a>/Shutterstock
This story originally appeared on the OnEarth website.
Carlos Jusino grew up a typical kid in Harlem, rollerblading near the Hudson River, eating at the McDonald’s on 145th Street and Broadway, hanging out with friends in his building. Also typical was the fact that many of Jusino’s neighbors and family members, including his mother, had asthma. “When I was growing up, she went to the hospital about once a month for asthma,” he says. Although he didn’t know it at the time, more than 30 percent of the kids in Harlem have asthma, one of the highest rates in the country.

Jusino’s family was worried about the air quality around Harlem, but most of its attention was directed to a sewage treatment facility built in 1985 along the West Side Highway next to the Hudson, where a foul-smelling settling tank lay exposed. The plant galvanized the community, including a group of environmental justice activists known as the Sewage Seven. They sued the city and won a settlement in 1994 that helped establish air-monitoring stations around the plant.
Harlem is plagued by health conditions not uncommon among the urban poor. In addition to suffering from asthma, children here have high rates of obesity and, perhaps most alarming, significant learning disabilities. Increasingly, medical researchers are discovering that all of these syndromes are linked at least in part to environmental factors, from nutrition to tobacco smoke to industrial chemicals. Jusino, like many, was stunned to learn that pollution’s biggest target may be not our lungs but our brains.
Researchers are finding the Harlem population to be a valuable source of data, and what they’re learning is both illuminating and worrisome. And if you think poor air quality is limited to disadvantaged urban neighborhoods, think again. Harlem’s problems are shared by the rest of the country. If clues can be found here, the lessons can apply elsewhere.
As many as one in six children nationwide has a neurodevelopmental disability, including autism, speech and language delays, and attention deficit hyperactivity disorder. The Centers for Disease Control and Prevention estimates that ADHD alone affects 14 percent of children, although experts debate whether it may be overdiagnosed. In any case, the number of children needing special education services has increased 200 percent in the past 25 years. In a 2000 report, the National Research Council of the National Academy of Sciences estimated that 3 percent of brain disorders are caused outright by environmental toxicity and an additional 25 percent by environmental exposures interacting with genetic susceptibilities.
Every day, America’s pregnant women and young children are exposed to a trifecta of suspected neurotoxicants in the form of pesticides (mostly via food and water but also home, lawn, and farm applications), polycyclic aromatic hydrocarbons, or PAH (mostly via exposure to vehicle exhaust), and polybrominated diphenyl ethers, or PBDEs (flame retardants, mostly in upholstered furniture and electronics). The CDC routinely samples Americans for these and other industrial by-products in our bodies, so we know their reach is pervasive. But we are not all equally exposed, and some of us appear to be more vulnerable to them for reasons that may include genetic susceptibility, poor nutrition, stress, and age.

Jusino joined a youth group through his high school in Washington Heights in 1994 and started mapping, block by block, local sources of pollution, including dry cleaners and diesel-spewing bus depots. In 1997 he joined the staff of West Harlem Environmental Action (We Act), a group co-founded by Peggy Shepard, one of the Sewage Seven. Today, as a GIS mapping specialist and technician, he is the proud chief caretaker of Aethan, a retro-looking black box that records real-time black carbon pollution. The size of a microwave oven, the Aethalometer (from the Greek word meaning “blacken with soot”) sends out several feet of PVC pipe through a window overlooking the corner of 152nd Street and Amsterdam Avenue, where the We Act offices occupy a light-filled, redbrick former police precinct house.
Aethan looks retro, but he has a Twitter account, where he says things like “Holy pollution, Batman! Look, the WE ACT Aethalometer reading is at 2,780 nanograms per cubic meter.” (For perspective, during low-traffic weekends, the readings hover around 1,200.)
“The readings get really high around 3:00 p.m.,” said Jusino, who, at age 35, sports silver-rimmed glasses and a trim goatee. Outside, it was early evening, and the machine was reading in the mid-700s. I couldn’t help imagining dark whorls of goblin-faced spirits wafting up to choke us at the windows. It’s a misconception, though, that the worst air pollution is visible. We tend to equate it with smog. Smog exists, of course, but it was largely knocked back under the air-quality controls of the 1970s. Over its 40-year life, the Clean Air Act has radically cut many ingredients of smog: carbon monoxide emissions are down 82 percent, sulfur dioxide 76 percent, and ozone concentrations 28 percent.
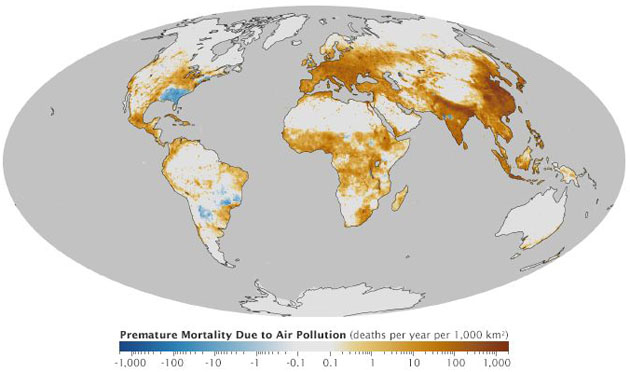
However, there are virtually no regulations governing the black carbon component of fine particulate matter smaller than 2.5 microns, known as PM 2.5. Black carbon is responsible for two million premature deaths globally each year. It also contributes substantially to climate change. A recent study by a team of 31 geophysicists found that black carbon is “the second most important human emission in terms of its climate forcing in the present-day atmosphere.”
Black carbon is a component of particulate matter left over from the incomplete combustion of fuels in vehicle engines, apartment-building boilers, cooking stoves, and other sources. Aethan’s 3:00 p.m. peak is the product of diesel-powered vehicles, including school buses. Harlem has one of the highest levels of black carbon in New York. In part, this is because of the high density of older buildings, which tend to have older, less efficient, and poorly maintained heating systems. But diesel fuel is also a major source of black carbon, and Harlem is home to six of Manhattan’s seven transit bus depots as well as commercial trucking routes. By 2006, after a big public campaign spearheaded by the Natural Resources Defense Council (NRDC), city transit buses that had previously used dirty diesel switched to a combination of filters and cleaner fuel. But plenty of other fleet vehicles, older school buses, and ships passing close by still burn the bad stuff.
A host of ills has been attributed to fine particulate pollution, including heart and lung disease, sometimes causing premature death. Black carbon is considered a reliable co-conspirator of PAH, a class of compounds that are also by-products of combustion. (Black carbon is easier to measure than PAH and, depending on location and source, tends to be highly correlated with them.) When inhaled, fine particulates go deep into the lungs, but they also travel to the brain, where they can alter DNA expression, cause inflammation, and possibly gum up neuronal circuitry. Jusino and others wondered: Could these and other common contaminants be contributing to the high incidence of neurodevelopmental delays in the children of Harlem?
* * *
Northern Manhattan is home to not only some of the best music, soul food, and dance troupes in the city but also one of its most venerated medical research institutions, Columbia University Medical Center. Frederica Perera was a young cancer researcher there in the 1980s when she decided to collect tissue samples from human placentas, expecting that they would be “pristine,” or untouched by environmental exposures. “But we found there were fingerprints on these samples of DNA damaged by pollution, even in women who weren’t smokers,” she recalled from her office at the Columbia Center for Children’s Environmental Health on West 168th Street. “It made me concerned about fetal exposures. I really wanted to look more closely at this window.” Although she started out looking for cancer markers, she was soon curious about other pressing health conditions in the Harlem community.

That Perera was even looking at environmental causes of illness was both unusual and unfashionable. For the past two decades, cancer researchers and other molecular biologists have spent much of their time riveted by the genome, believing it would unlock the secrets of disease. But cellular life isn’t determined simply by the blueprints of DNA. It’s now understood that cells are designed to interact nimbly with the outside world and that genes get turned on or off—and are sometimes mutated altogether—by environmental exposures from diet, inhalation, even transmission through the skin. To truly understand human health and disease, scientists need to look at both the genome and—to use a term coined in 2005 by Christopher Wild, a cancer epidemiologist—the “exposome.”
Perera decided to do just that.
Today, as director of the Columbia center, she oversees what has become one of the most respected epidemiological data troves in the country. (She is also a trustee of NRDC.) Starting in late 1998, Perera and her colleagues recruited more than 700 pregnant women from hospitals in Harlem, Washington Heights, and the South Bronx for what’s known as the Mothers and Children Study. Now, 15 years later, the team has retained three-quarters of its original participants, and the first babies are entering their teenage years. Such “prospective” studies, which follow a group over time and measure their health outcomes, are considered the gold standard in scientific research because they don’t rely on retrospective memory or old, imperfect medical records. Blood and urine samples have been banked since the mothers’ pregnancies and deliveries, as have samples from the children, and researchers can go back to these as they ponder new questions.
It’s now known that many chemicals can cross the placenta, once believed to be a sacrosanct barrier. This is disquieting, because the vast majority of these chemicals have never been tested for human health effects. Furthermore, the medical community agrees that many diseases and conditions, including obesity, cancer, and autism, are modulated by both genes and fetal exposures. In September, the American College of Obstetricians and Gynecologists and the American Society for Reproductive Medicine issued a joint statement saying, “The scientific evidence over the last 15 years shows that exposure to toxic environmental agents before conception and during pregnancy can have significant and long-lasting effects on reproductive health.” (The chemical industry, however, is seeding doubt. The American Chemistry Council’s chief medical officer responded that ACOG’s evidence was based on “a limited number of flawed studies.”) It makes sense to developmental biologists that fetal exposures matter; this is when the cells in the body and brain are on the biggest adventure of their lives, differentiating and replicating like a one-way train. Once it’s left the station, it doesn’t go back.
Children, of course, are harder to study than lab animals, because they are exposed to so many different conditions that can confound the results. That’s why large, prospective epidemiological studies are so critical. Perera knows both what’s in these babies’ bloodstreams and what happens to them as they age. The larger the study, the stronger the statistical power. Even so, epidemiological findings are necessarily couched in terms of “associations” rather than causal links. So epidemiologists often look to better-controlled animal studies as a guide, as well as to molecular lab investigations of human blood and tissue samples.
With enough replication and diverse strategies, a picture begins to emerge. The center’s early studies found significant associations between pollutants measured in the mothers and difficult birth outcomes, including low birth weight and small head circumference. The main culprits were PAH and chlorpyrifos, a then-common organophosphate pesticide used indoors to kill roaches and bedbugs. (Later the team would look at flame retardants.) Perera also documented that these chemicals damaged cellular DNA. Chlorpyrifos was found in the umbilical cords of virtually every mother in the early samples. Since 2001 it has been phased out of residential use, but exterminators are still caught using it. It also remains a common agricultural pesticide and so ends up as a residue in food. Perera and her colleagues knew that reduced head circumference had been linked to lower IQ scores, and animal experiments had shown that chlorpyrifos killed developing brain cells and induced behavioral changes in rats. In some well-known experiments, for example, rats given low doses of the pesticide while in the womb or shortly after birth later had trouble learning their way around a maze.
Although Perera and her team didn’t know how these chemicals might be changing the brain, they were determined to find out all they could about the children’s growth and development. The children (now teenagers), who are mostly Dominican and African American, would be regularly tested on everything from reading ability and motor skills to psychological yardsticks like aggression, risk-taking, and depression.
By the time they were 3 years old, the children with the highest exposures to the pesticide tested as much as six points lower on motor skills and three points lower on mental development and were significantly more likely than those with lower exposures to suffer from attention and hyperactivity problems. These findings were published in 2006 in Pediatrics. Other studies showed that children most exposed to PAH were nearly three times as likely to show cognitive developmental delays. By the time they were 7, the children most exposed to chlorpyrifos were showing deficits in working memory, a key component of IQ. Their working memory declined by 2.8 percent and their full-scale IQ by 1.4 percent, after adjusting for variables like tobacco smoke and maternal intelligence.
The center’s findings on the cognitive impacts of PAH and pesticides bolster what other researchers have found in Boston, Cincinnati, and California. Perera led a similar cohort study with researchers in Poland and found that higher prenatal exposure corresponded to an average 3.8-point drop in IQ in 5-year-olds. This drop is comparable to the effects of lead, the discovery of which, in the 1970s, eventually triggered a massive public health response in the form of laws removing lead from automobile gasoline, restricting it in household paint, and, to this day, requiring lead tests in children in many parts of the country.
Now that the Harlem children are older, the team is examining whether the ill effects of fetal and cumulative exposures play out in other ways—poor academic performance, impaired social skills, anxiety and depression, and self-destructive behavior.
On the day I visited the center this fall, a mom—let’s call her Michelle—and her 14-year-old son came in for a couple of hours of assessments. They were both greeted by a tremendous hug from Diurka Maria Diaz, a researcher and counselor who has followed the families from the beginning. “You’re taller than I am now!” she teased the boy. Hefty, dressed in black pants and a black sweatshirt, he towered over his toddler sister. She is also in the study, which continues to recruit new participants who likely have different exposomes. While Michelle’s placenta absorbed chlorpyrifos during her son’s gestation, it probably absorbed replacement pesticides during her daughter’s. The replacements come from a class of chemicals known as pyrethroids, whose neurodevelopmental effects remain largely unstudied.
Diaz, who is known to the families as Didi, exudes warmth and charisma as well as concern for the challenges faced by kids in the study. “It’s hard to be a 14-year-old,” she says. “Many of these kids are overweight, many are depressed. We’ve referred about 40 percent for counseling.” Furthermore, a remarkable 24 percent of the cohort children at age 2 had a potentially diagnosable developmental delay. About 70 percent of these children qualified for New York City’s early intervention services.
Such delays are typically attributed to growing up in impoverished environments with relatively low parental involvement, low mental stimulation, and pervasive psychological stress. Perera’s team, though, is convinced that fetal environmental exposures play a role and that their effects may be aggravated when combined with maternal stress, as well as when combined with one another.
“In the past, we took a reductionist approach,” Perera says, “a single exposure, a single effect. But now we think that pollution interacts with nutritional and social susceptibility factors. We’re making heroic attempts to measure these. We’re building the exposome.”
The environmental trail of brain damage extends far back in history. Accounts of lead toxicity date to the Greek physician Nicander of Colophon in 200 B.C. In more recent times, a French physician in 1848 described ill-tempered infants who’d been sucking on lead soldiers. More examples of damaged childhoods came to light after twentieth-century commercial and industrial exposures. A cheap, arsenic-laced stabilizer was added to powdered milk in Japan during the spring of 1955, causing sickness, epilepsy, or lowered IQ in more than 12,000 victims, most of them infants. (Studies of nerve cells in a Petri dish suggest that arsenic inhibits cell growth and, in the developing brain, reduces the branching of dendrites—the structures of neurons that send and receive signals.) Also in the 1950s, a factory in Minamata, Japan, began releasing mercury into the local bay, ultimately causing severe physical and cognitive problems in children whose mothers ate contaminated fish while pregnant.
By the mid-1970s researchers around the world had documented cases of lowered IQ in children exposed to lead from air pollution, mercury-based preservatives in grain, and polychlorinated biphenyls (PCBs) in fish, as well as in those exposed to alcohol in utero. The effects were much greater in children than in exposed adults. These were, as the neurotoxicologist Pam Lein of the University of California, Davis, puts it, “the blunt ones”—exposures whose effects became apparent after some concerted research. But no one really understood how the toxins worked, and they didn’t know if other, more subtle, discoveries awaited.
In 1972, a Danish medical student named Philippe Grandjean saw a young woman on television who was suffering from so-called Minamata disease. Exposed to mercury in the womb, she could hardly talk and was afflicted by a severe spastic limb condition. Grandjean wondered why he wasn’t being taught about environmental exposures if they could cause so much damage. He decided to spend his life researching neurotoxicants, which he terms “brain drainers.” Since then he has written more than 100 papers on mercury, taught a couple of generations of scientists, and as both a physician and a researcher has an understanding of the micro and macro scope of the problem. What he told me wasn’t comforting.
“Because the human brain is so complex, it’s incredibly vulnerable,” says Grandjean, now an adjunct professor at the Harvard School of Public Health and the author of the 2013 book Only One Chance: How Environmental Pollution Impairs Brain Development and How to Protect the Brains of the Next Generation. “Even if something goes a little bit wrong, you don’t get a second chance,” he says. “You’re stuck with it, and even small deficiencies can be quite significant.”
As Grandjean explains it, shortly after conception, the brain begins to form from a tiny strip of cells. At its fetal growth peak, 12,000 cells are generated every minute, or 200 per second. These cells start sending and receiving messages and migrating to specific locations. By the time the brain is fully baked, it has close to 100 billion nerve cells and roughly as many caretaking glia cells, which provide nutrients, sweep out dead cells, and insulate nerve fibers. “If cells are in the wrong place or they don’t form the right connections,” Grandjean says, “that’s what you’ve got for your whole life.”
In a groundbreaking review published in the Lancet in 2006, Grandjean and his co-author, Philip Landrigan, of Mount Sinai Hospital in New York City, identified 201 heavy metals, solvents, pesticides, and endocrine disruptors known to have toxic effects in the human brain (at least 1,000 other substances are neurotoxic in animals but haven’t been tested in humans). Of those 201, about half are “high production volume” chemicals, made in or imported to the United States in excess of one million pounds per year. At the time, the authors could point to only half a dozen as showing evidence of developmental toxicity in the fetal brain, but the count is now up to 10 and growing. All of these neurotoxicants are relatively common, routinely found in the blood of pregnant women. They include the usual suspects—lead, methylmercury, and PCBs—but also organochlorine pesticides like DDT (which was banned in the 1970s but still persists in soil and water), organophosphate chemicals like the roach-killer chlorpyrifos, PAH, PBDEs (this pervasive class of flame retardants is now being phased out), arsenic, ethanol, and the solvent toluene.
We are beginning to learn more about how these substances may alter brain development. Their strategies are complex and varied. Under the influence of methylmercury, for example, the brain’s nerve cells “are lying helter-skelter, not in their usual logical locations,” says Grandjean. Pesticides are designed to be neurotoxicants—that’s the whole point—and some, like chlorpyrifos, work by inhibiting cholinesterase, an enzyme critical to brain-cell communication. Different neurotoxicants affect children differently. At high levels, methylmercury appears to cause memory deficits, while lead primarily decreases attention span and pesticides tend to impair spatial perception. Black carbon apparently affects attention and processing speed.
Not all kids are equally vulnerable. Other factors matter, like genes, psychosocial stress, and, interestingly, gender. Boys tend to be more vulnerable than girls to the deficits associated with PAH. Studies of prenatal exposures to phthalates and bisphenyl-A (BPA), both endocrine disruptors, also show gender differences. Phthalates are considered anti-androgens, while BPA acts like an estrogen, and the developing brain takes important cues from both hormones. With chlorpyrifos exposure, for example, boys have greater difficulty than girls with working memory.

Many of these substances disproportionately affect the poor, but not all. Poor kids are exposed to more lead and first- and secondhand tobacco smoke. More affluent populations accumulate more mercury from their diet. Urban kids may be exposed to more PAH and black carbon, farm kids to more pesticides and arsenic from well water.
Of all the suspects, brominated flame retardants may be the most democratic. Although levels of PBDEs are now dropping in pregnant women, Americans still have the highest levels tested anywhere in the world. Flammability standards enacted in California in the 1970s resulted in the addition of PBDEs to everything from electronics to home furnishings nationwide. Unfortunately, the molecules easily migrate, accumulating in blood and breast milk and persisting for years. Structurally similar to PCBs in some cases, they appear to interfere with thyroid hormone signaling, either by directly altering the amounts of hormone or by blocking the hormone transporters. As researchers learned from studying cretinism, thyroid hormones are critical to brain development, among other functions.
A University of California, Berkeley, study of children in the state’s Salinas Valley reported that those born to mothers with the highest levels of PBDEs during pregnancy averaged six points lower in verbal IQ and had lower scores for fine motor skills and a higher risk of hyperactivity. And PBDEs probably don’t act in isolation. Per Eriksson, a Swedish toxicologist, has found that when lab animals are exposed to both PBDEs and mercury, the neurological effects are significantly stronger than those of mercury alone.
Philip Landrigan directs the children’s environmental Health Center at Mount Sinai Hospital. Like Grandjean, he is a pillar in the field; in the 1970s, he linked childhood IQ deficits to low levels of lead. More recently he’s been integral to health studies of rescue workers who were exposed to toxic particles during 9/11. Caps from the New York City police and fire departments and the US Navy decorate his office on East 102nd Street.
What worries Landrigan is how easily many neurological effects can fly under the radar. These are not the kinds of acute poisonings that land kids in emergency rooms. Most doctors are not trained to look for prenatal or childhood environmental exposures. If parents ask them about it, he says, “they tend to offer bland reassurance.” But for the individuals and families involved, learning, psychological, and behavioral impairments can have dramatic, lifelong impacts on meaningful measures from happiness to income.
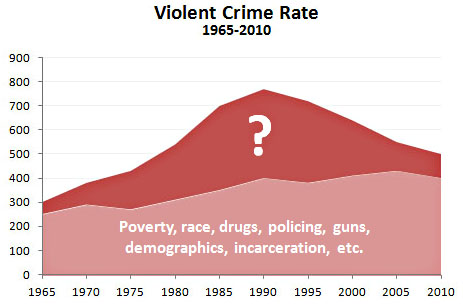
But do a few IQ points matter? Should society care if a boy behaves a few shades more or less aggressively? These are questions that currently interest epidemiologists more than family physicians. One of Landrigan’s associates at Mount Sinai, research scientist Megan Horton, who worked previously with Perera, told me that an average drop of five IQ points in the United States translates into 2.4 million gifted kids instead of 6 million, and 9.4 million mentally retarded children instead of 6 million, or a 57 percent increase. Leonardo Trasande, a pediatrician formerly at Mount Sinai and now at the New York University School of Medicine, has estimated that mercury exposures alone have led to losses of 0.59 to 3.2 IQ points in several hundred thousand children born every year in the United States, resulting in decreased lifetime economic productivity valued at $8.7 billion annually. Thanks in large part to the laws spurred by Landrigan’s epidemiological sleuthing, airborne lead pollution has declined 90 percent since 1980. With the decline has come a concomitant improvement in IQ scores and an intriguing drop in youth aggression and urban crime.
Landrigan argues that the field of environmental health must become a centerpiece of public health. Mount Sinai has one of just 11 children’s environmental health centers nationwide. He’s disappointed that Congress last year pulled substantial funding from the once-promising National Children’s Study, which aimed to follow the exposures and health of thousands of children. At the same time, federal legislation that would strengthen the way chemicals are tested and regulated gets repeatedly stalled.
“Clearly there’s a need for a new regulatory apparatus for testing chemicals, and the backlog is huge,” says Miriam Rotkin-Ellman, a senior scientist specializing in public health at NRDC. “There are also a lot of gaps in the science, both in terms of characterizing the health end points, such as autism, and in terms of understanding the mechanisms by which chemicals can interact with neurodevelopment. What’s the timing and what are the pathways of exposure?”
Recognizing the need for more data, Landrigan’s program is about to launch its own $20 million prospective study following children from the womb through childhood. It will complement the work being done at Columbia and also at the University of Utah. “We will in some instances combine and pool our data in order to increase our ability to discover links between environmental exposures and disease,” says Landrigan.
Meanwhile, Perera’s group has embarked on the next frontier in environmental health: brain imaging. Now that Columbia has data on exposures and cognitive problems, it makes sense to look at the brain structures themselves. Have the chemicals altered the brain in physically obvious ways?
In a nutshell, “yes,” says Virginia Rauh, a perinatal epidemiologist at Columbia. Brain images of 5- to 11-year-olds with the highest exposures to chlorpyrifos show subtle deformations in parts of the brain associated with receptive language and social cognition and a thinning of areas of the parietal and frontal cortices, which are involved in executive functions like attention and problem solving.
Using brain imaging to complement large-scale epidemiology is brand new. It’s also very expensive, and the technology is still being validated. Although Rauh admits that her team is “far from being able to say these changes are linked to impairment,” it’s time to focus on that question. “Public health has not really looked at the brain, other than with metals like lead and mercury,” she says. “Our challenge is to link particular deficits we’re seeing to meaningful impairment so that we can intervene and prevent them.”
I took the train back home to Washington, DC, passing through the northeast corridor’s confused, tight mix of commercial promise and marginalized decay. Over it all hung the molecular by-products of progress. To get a sense of just how far black carbon reaches into my own family’s life, I decided to take a cue from Jusino and his pet Aethan and order up my own air-monitoring companion for a few days. I called Steven Chillrud, co-director of the Exposure Assessment Facility Core at Columbia’s Lamont-Doherty Earth Observatory. An environmental geochemist, he tries to figure out how much black carbon people are exposed to by strapping carbon-measuring machines to buildings and sometimes car commuters, pedestrians, and bicyclists. He FedExed me a loaner micro-Aeth patched into a twill vest. I decided to call it Aethchyluth, honoring the urban Greek tragedian with a lisp. Aside from a few lumps, the device was fairly unobtrusive. No one seemed to notice the small sensor stretching upward toward my chin like a playful pet monkey. I wore it for most of three days while walking and driving around Washington in my daily routine.
After I shipped Aethchyluth back, Chillrud sent me the data graph, which looks like an EKG reading, drawn in thin blue spikes. Then we matched the graph to the record from a GPS app, which had tracked my travels. High spikes occurred on I-495, the Capital Beltway, which wasn’t a surprise. Although I avoid it like the plague at peak rush hour, I’d driven it a couple of times at off-hours to visit relatives in southern Maryland. Even in my car with the windows rolled up, my levels hovered around the 6,000 nanograms per cubic meter mark, or more than twice the average reading Jusino was getting on his Harlem corner on a typical weekday.
I pitied the people who drive this twice a day in slow-moving traffic, but they don’t get the most sympathy from Chillrud. “Schools and day-cares are typically built on the cheapest land, often next to highways,” he says. “That’s where developing lungs are, and susceptible kids.”
But as my readings made clear, schoolchildren don’t need a major freeway to breathe in black carbon and PAH. Aethchyluth got readings equal to the beltway in the parking lots at my kids’ schools. That’s because idling cars and school buses sit there just as kids are leaving. I was reminded of what a neuroscientist who studies brain inflammation told me: “I hold my breath when I’m behind a diesel bus.”
Nineteen percent of Americans live near high-volume roads, and most areas don’t monitor the air. So just how bad were my readings? We don’t really know, says Chillrud, because the EPA hasn’t issued guidelines for black carbon pollution the way it has for other pollutants. Black carbon is complicated because it’s a proxy for many pollutants, he explains, and there are no consistent ways to measure it. In the meantime, city and federal officials recommend we reduce it through the use of cleaner fuels, newer engines, and, in New York City’s case, mandated higher-quality fuel oil. “It will gradually get better,” he says. “But there’s still a lot to do.”
When I was in Harlem, Frederica Perera had laid out a busy future of continued studies of childhood exposures to everything from PAH to phthalates to BPA to the newer pyrethroid pesticides. Her windows looked out over the Hudson River, a reminder of our collective interdependence on the air and water that both nourish us and transport pollution into our cells. The river glinted as it flowed out to sea. Once ragingly filthy, it is now cleaner than it has been in two generations.
Policy changes work, and some of those changes are quickly mirrored in our bodies. After the residential phaseout of chlorpyrifos, levels in pregnant women fell significantly. A small study published in September in the journal Environmental Science and Technology found that levels of some brominated flame retardants in pregnant Californians were 65 percent lower than in a similar group tested three years earlier (a phaseout began in 2004). By 2006, after converting to cleaner fuel and using filters, New York City’s transit buses reduced their emissions of particulate matter by 97 percent.
“If the science is utilized well, policy makers can act. That’s why it is enormously helpful,” said Perera. “The good news is that by nature these exposures are preventable.” She stood up to go to a meeting, passing framed photos of four of her grandchildren. On her way out she sent a warm greeting to Michelle. More families would be arriving soon.