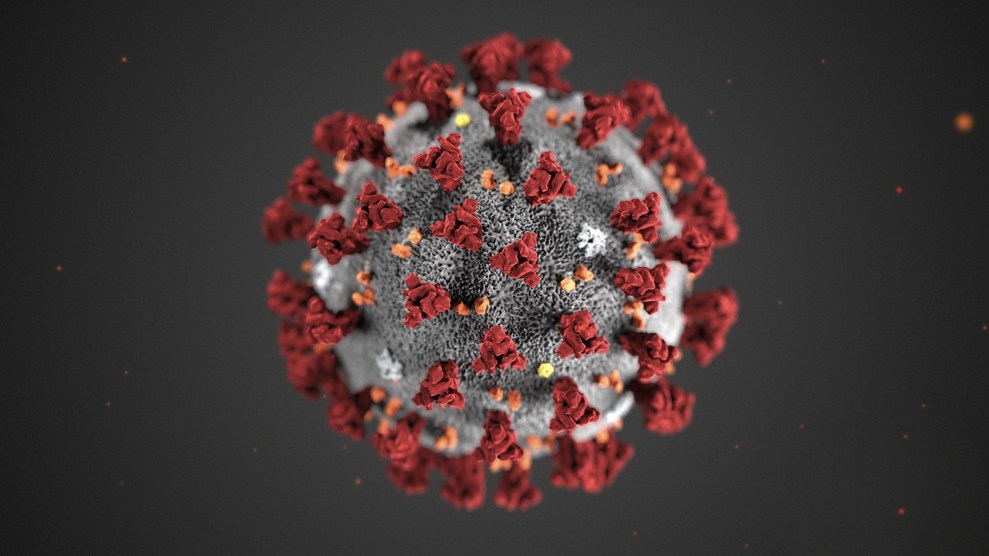
CDC/Planet Pix via ZUMA
The more we learn about COVID-19, the worse it gets. This is from a recent study of recovered patients in Germany:
CMR [cardiovascular magnetic resonance] revealed cardiac involvement in 78 patients (78%) and ongoing myocardial inflammation in 60 patients (60%), independent of preexisting conditions, severity and overall course of the acute illness, and time from the original diagnosis.
Nearly two-thirds of patients, even those with no preexisting conditions, developed myocarditis! Now, myocarditis is not always serious, but it can be. Sometimes it lasts a few hours, other times a few months. But why is a respiratory virus causing heart problems? The good folks at UCSF magazine explain:
We Thought It Was Just a Respiratory Virus
We were wrong.By the luck of the evolutionary draw, [the coronavirus can] easily grab hold of protein gates on human cells known as ACE2 receptors and, like jackknives, pry these gates open….“You can think of an ACE2 receptor like a docking site,” says Faranak Fattahi, PhD, a UCSF Sandler Fellow.
….It stands to reason that SARS-CoV-2 affects the heart. After all, heart cells are flush with ACE2 receptors, the virus’s vital port of entry. And, indeed, laboratory experiments suggest that the virus can enter and replicate in cultured human heart cells, says Bruce Conklin, MD, a professor of medicine and an expert in heart-disease genetics at UCSF and the Gladstone Institutes.
This, along with interactions from the immune system, appears to be responsible for many of the non-respiratory effects we’ve started seeing in COVID-19 patients. That’s why, increasingly, it’s not just important to get COVID-19 deaths down. We need to crush the case count too because even seemingly asymptomatic cases can sometimes cause serious problems down the line.