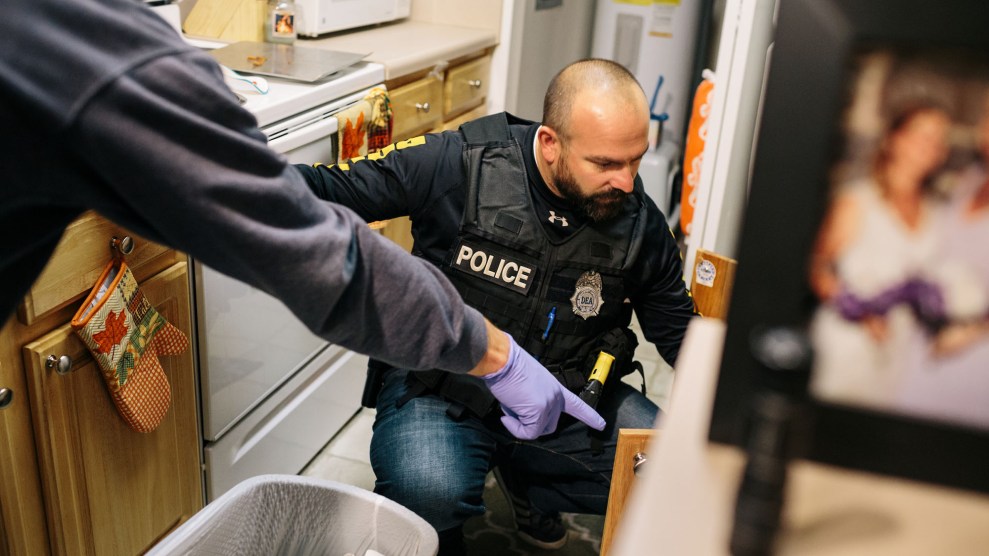
Richard Chenery injects heroin he bought on the street at the Insite safe injection clinic in Vancouver.Darryl Dyck/The Canadian Press/AP
On Tuesday, Philadelphia took a step towards becoming the first city in the country with a supervised injection facility—a controversial but evidence-based initiative that many say could be key to stemming the rising tide of opioid overdoses.
City officials announced that it would allow the sites, also known as “safe consumption facilities,” within the city limits, allowing drug users a clean, safe space to inject illicit drugs. The decision is not without controversy. While drug policy researchers point to studies showing that existing safe injection facilities (SIFs)—there are more than 100 in Canada, Germany, the Netherlands, and elsewhere—reduce drug overdoses, critics say the sites will enable drug use.
“No one here condones or supports illegal drug use in any way,” assured Philadelphia public health commissioner Dr. Thomas Farley, adding that SIFs are just one of many components of the city’s overdose prevention strategy. “We want people saddled with drug addiction to get help.”
SIFs are a prime example of what’s called harm reduction, or the idea of making drug use safer so that eventually, users seek treatment. (Needle exchanges, which provide clean injection supplies, and the distribution of naloxone, the overdose reversal drug, are others.) Each SIF looks different, but a typical facility is located in a neighborhood with concentrated drug use and consists of hygienic space for users to shoot up, clean needles and other injection supplies, access to naloxone, and supervision from nurses or others with medical training. Some sites also have a place for users to spend time as they’re coming down from the drug’s effects.
There have been hundreds of studies on the efficacy of SIFs, many of them on Vancouver’s Insite facility—the first such site in North America, where roughly 5,000 overdoses have been reversed since the clinic was founded in 2003. They’ve found that not only do SIFs reduce overdose deaths, but they reduce the transmission of infectious diseases like HIV and hepatitis C, increase access to addiction treatment, and save cities money in hospital and prison costs.
SIF proponents also argue that they reduce the publicity of drug use and its ripple effects. “There’s a terrific public nuisance benefit,” says Dan Ciccarone, an epidemiologist at University of California-San Francisco who studies the opioid epidemic. “You don’t have folks injecting on the streets or overdosed in front of businesses. It decreases defecation, it decreases discarded syringes, it decreases public sleeping and slumping and stuff like that.”
No US city has a SIF yet, but support is moving mainstream: Last year, the American Medical Association came out in favor of piloting the facilities in the United States. Seattle’s city council allocated $1.3 million for a site in November, and policymakers in many other cities—including San Francisco, Denver, and New York—have expressed support, but none have concrete plans to open facilities. That’s partly because SIFs aren’t particularly intuitive: San Francisco’s late mayor Ed Lee described a similar proposal as a “city-funded shelter” for residents to “literally destroy their bodies and their minds.” And then there’s the fear of law enforcement, particularly under Attorney General Jeff Sessions, who has taken a tough-on-crime approach to the epidemic so far. As Ciccarone put it, “The question is, ‘Will the feds come in and bust it?'” (For more on SIFs, check out my colleague Amy Thomson’s explainer.)
Philadelphia has an estimated 70,000 heroin users and one of the highest overdose rates of any city in the country. The city itself won’t operate the facilities, but rather it is soliciting operators interested in setting up the sites. A recent report conducted on behalf of the city’s health commissioner estimates that a SIF could prevent more than 70 overdose deaths a year, and could save millions of dollars.
“There’s a race going on and Philly just got to the front,” said Ciccarone. “As soon as one happens, you’re going to see a dozen.”